Abstract
Glaucoma is a common, complex, heterogenous disease and it constitutes the major cause of irreversible blindness worldwide. Primary open-angle glaucoma (POAG) is the most common type of glaucoma in all populations. Most of the molecular mechanisms leading to POAG development are still unknown. Gene mutations in various populations have been identified by genetic studies and a genetic basis for glaucoma pathogenesis has been established. Linkage analysis and association studies are genetic approaches in the investigation of the genetic basis of POAG. Genome-wide association studies (GWAS) are more powerful compared with linkage analysis in discovering genes of small effect that might contribute to the development of the disease. POAG links to at least 20 genetic loci, but only 2 genes identified in these loci, myocilin and optineurin, are considered as well-established glaucoma-causing genes, whereas the role of other loci, genes, and variants implicated in the development of POAG remains controversial. Gene mutations associated with POAG result in retinal ganglion cell death, which is the common outcome of pathogenetic mechanisms in glaucoma. In future, if the sensitivity and specificity of genotyping increases, it may be possible to screen individuals routinely for disease susceptibility. This review is an update on the latest progress of genetic studies associated with POAG. It emphasizes the correlation of recent achievements in genetics with glaucoma pathophysiology, glaucoma treatment perspectives, and the possibility of future prevention of irreversible visual loss caused by the disease.
Similar content being viewed by others
Introduction
Glaucoma is a major cause of irreversible blindness worldwide.1 It is defined as a group of complex disorders characterized by progressive degeneration of the retinal ganglion cells, resulting in characteristic visual field defects, which reflect optic nerve atrophy, with a distinctive clinical appearance.
Primary glaucoma occurs in the absence of an identifiable secondary cause (eg, pseudoexfoliation, pigment dispersion, chronic uveitis, and so on). Classification of primary open-angle glaucoma (POAG) is mostly based on the age of onset and therefore it is classified as primary congenital glaucoma (onset up to 3 years of age), juvenile open-angle glaucoma (JOAG/onset at 10–35 years), and adult-onset POAG (after the age of 35 years).2 The latter is the most common form and the one that does not follow a clear inheritance pattern.
Normal tension glaucoma (NTG) refers to patients with glaucoma, an open-angle, characteristic visual field defect and an intraocular pressure (IOP)<22 mm Hg without treatment.3
Several risk factors have been evaluated for POAG, including black race, untreated systolic hypertension, current cigarette smoking, family history of glaucoma, diabetes mellitus, and myopia.4 Elevated IOP was found to be a major risk factor.5 An interaction between genetic and environmental risk factors is usually assumed to confer the complex disease phenotype.6
Family studies have shown the contribution of genetic variation to the development of the disease.7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 Relatives of POAG patients have a 22% risk of developing glaucoma at some point in their lives, whereas the risk for the relatives of the normal controls is 2–3%.18 Gene variants, discovered so far, predisposing to glaucoma, may together contribute up to 5% of all POAG and NTG cases. Therefore, 95% of the genetic contribution for POAG remains undetermined.
Further identification of the genetic basis of glaucoma should help delineate the pathogenesis of the disease. This in turn may identify novel therapies and/or drug targets. Ultimately presymptomatic genetic testing and preventative treatment may be possible.
This review focuses on current knowledge and latest breakthroughs in POAG genetics. It aims to provide a comprehensive analysis of how known genetic variations associated with POAG might ultimately result in the clinical phenotypes noted in POAG. It also assesses how such understanding may lead to novel therapeutic interventions for POAG.
Search strategy
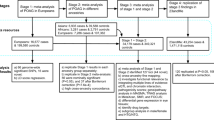
We searched the MEDLINE/PubMed database for articles from August 1987 to June 2011, after following the MeSH suggestions for articles including the terms: ‘primary open glaucoma’, ‘glaucoma pathogenesis’, and ‘genes in glaucoma’. The headline used to locate related articles in PubMed was ‘glaucoma genetics’ and to restrict the search, we used the headlines ‘genes and pathogenesis of primary open-angle glaucoma’, ‘genome-wide association studies (GWAS) in primary open-angle glaucoma’, and ‘gene therapy in primary open-angle glaucoma’. A manual search was also based on references from these articles, as well as review articles.
Genetic terms and approaches
A classical Mendelian inheritance pattern is one in which a genotype at one locus is both necessary and sufficient for the phenotype to be expressed.19 Glaucoma, however, is characterized as a ‘complex’ disease. That is a phenotype that exhibits heterogeneity, polygenic inheritance, phenocopies, and incomplete penetrance.20
‘Genetic heterogeneity’ indicates that different genes or different genetic mechanisms are involved in different pedigrees. Clinically, genetic heterogeneity refers to the presence of a variety of genetic defects causing the same disease.21
‘Polygenic inheritance’ refers to traits, which are influenced by multiple genes.
‘Incompete penetrance’ means that some individuals fail to express the trait, even though they carry the allele. ‘Phenocopies’ refers to individuals whose phenotypes are the cause of enviromental factors and are identical to the ones whose phenotype is determined by the genotype. Thus, the genotype at a given locus may affect the probability of disease, but not fully determine the outcome.20
Although glaucoma exhibits all the above features, traditional linkage analyses have been widely used to identify linkage of different forms of glaucoma to particular loci. ‘Traditional linkage analysis’ utilizes one or more families with multiple members affected. To obtain a statistically significant result, typically greater than 10 affected individuals are required in a three-generation family to generate a logarithm of the odds score of >3, which equates to a P-value of 0.05. This generally results in identifying a large chromosomal region within which the causative gene resides. The gene then may be identified by a process of selecting candidate genes from within the region and assessing whether a plausible mutation is detected in the gene, which (a) segregates with the phenotype in the family and (b) is found to be mutated in other patients affected with the same disease. The myocilin (MYOC) gene was identified via this approach of positional cloning.11, 13
However, the traditional candidate gene approach can be inadequate for diseases with an unclear pathophysiology.22 Another method to identify genes contributing to complex diseases is genome-wide association.23
Association studies are case–control studies, based on a comparison of unrelated-affected and -unaffected individuals from a population.20 The aim is to determine the statistical associations between common genetic variations within the human genome and disease. This type of analysis is based on single-nucleotide polymorphism (SNP) arrays. SNPs are the most common type of genetic variation among people and each one represents a difference in a single nucleotide. On average, SNPs occur at a frequency of 1 DNA base in every 1000 throughout a person's DNA. When SNPs occur within a gene (when they fall within coding sequences of genes) or in a regulatory region near a gene, they may have a more direct role in disease by affecting the gene's function. They can act as biological markers, helping scientists locate genes that are associated with disease. Common chronic disease-associated genetic variants were identified by investigators using this approach in cancer, Crohn disease, and other common, chronic diseases.24, 25, 26, 27 Indeed, age-related macular degeneration (AMD) was one of the first ‘complex diseases’ in which genetic variants were successfully identified by genome-GWAS.23 A couple of recent GWAS for POAG have identified sequence variants and genetic loci associated with POAG susceptibility in populations of European and East Asian ancestry.28, 29
The advantages of GWAS include the fact that a specific disease model is not needed, which can allow identification areas of previously unsuspected pathogenesis. It seems likely that pathogenesis of most cases of glaucoma, excluding those in which single gene defects have been identified, may be due to contributions from many different polymorphisms. Thus, the likelihood of picking up an association is going to depend on the ability to control for errors induced by bias and poor phenotyping. Therefore, careful phenotyping is likely to be critical. However, large numbers of cases and controls are needed, and a particular challenge will be to identify the biological context in which statistically significant candidate variants act. This may reflect linkage disequilibrium (non-random combinations of alleles or genetic markers in a population more often or less often than would be expected from a random association of alleles) between the SNPs identified and the true causative functional variant. Therefore, identification of significant SNPs by GWAS needs to be followed up by fine mapping of the regions harboring the most significant statistical signals. This has significant cost implications.
It was thought that SNPs in DNA were the most prevalent and important form of genetic variation. However, recent studies30, 31, 32, 33, 34, 35, 36, 37 reveal that a major source of variation between individual humans, underlying human evolution and many diseases is another form of structural variation called copy number variations (CNVs) or copy number polymorphisms, which are DNA alterations that result in cell having an abnormal number of copies of one or more sections of the DNA. Genes that were thought to always occur in two copies per genome have now been found to sometimes be present in one, three, or more than three copies. Notably, the copy number variable regions encompassed more nucleotide content per genome than SNPs, underscoring the importance of CNV in genetic diversity and evolution.38
CNVs may be pathogenic in a variety of human diseases, including POAG.39, 40, 41
Advances in biochemistry, chemistry, and engineering have enabled the development of new gene expression assays.42 High-capacity systems can measure the expression of many genes in parallel, instead of studying one gene at a time. Leung et al43 demonstrated that microarray technology could contribute to the understanding of glaucoma pathogenesis in their investigation of differential gene expressions of an established human trabecular meshwork (TM) cell line under dexamethazone treatment. Similarly, Johnson et al44 used microarray analysis to identify gene expression changes in the pressure-injured optic nerve head (ONH) in a rat glaucoma model. They found that the most significantly affected gene classes were cell proliferation, immune response, lysosome, cytoskeleton, extracellular matrix, and ribosomal. Their study provides an opportunity to identify early gene changes that may have an important role in the pathogenesis of axon damage. By identifying these genes, they expect to identify specific processes by which the stress resulting from elevated IOP is translated to axonal injury within the ONH.
Genetic loci and glaucoma-associated genes
POAG links to at least 20 genetic loci.45 Among them, 14 chromosomal loci have been designated GLC1A to GLC1N by the HUGO Genome Nomenclature Committee (http://www.genenames.org/; ‘GLC’: glaucoma, ‘1’: primary open angle, ‘A to N’: chronological order of genes discovered; 5 of them (GLC1A, GLC1J, GLC1K, GLC1M, and GLC1N) contributed to JOAG, whereas the others contributed only to adult-onset POAG. Only three genes causing POAG, MYOC, optineurin (OPTN), and WDR36, have been identified in these loci, that is, in GLC1A, GLC1E, and GLC1G, respectively.9, 13, 46 Rare mutations associated with POAG in a novel gene, neurotrophin-4 (NTF4), have been recently identified in a European, as well as in a Chinese population.47, 48
A review of the literature on glaucoma genetics suggests a useful separation of them into those which are well-established glaucoma-causing genes, controversial genes that do not have an established role in glaucoma pathogenicity at present, and low-penetrance risk alleles that contribute to the likelihood of getting disease, but don’t cause disease on their own.
High-penetrance glaucoma-causing genes: MYOC and OPTN
TIGR/MYOC gene at the GLC1A locus
Sheffield et al11 studied 37 members of a Caucasian family in the United States with a history of an autosomal dominant form of JOAG and 22 were found to be affected. Linkage analysis mapped the disease-causing gene to chromosome 1q21–q31, which was named GLC1A. GLC1A was also linked with late-onset POAG.49
In 1997, Stone et al13 discovered the first gene, in which mutations were identified to cause JOAG, mapping to the GLC1A region. Among several genes mapping to this region and considered as candidates for the disease-causing gene, they screened two for mutations in families with JOAG, APT1LG1 (apoptosis antigen ligand 1) and TIGR (TM-induced glucocorticoid response protein), and they found compelling evidence that mutations only in the TIGR gene were responsible for the disease. TIGR was later known as the MYOC protein and the TIGR gene as the MYOC gene.
More than 70 mutations in the MYOC gene in different racial/ethnic populations, in animal models, and in cell cultures have been found to contribute to the pathogenesis of POAG, and numerous SNPs causing or not causing glaucoma have been reported.50 MYOC glaucoma is the most common form of inherited glaucoma (2–4% of glaucoma worldwide).51 Of note, it is particularly associated with high IOP in both the early and the later onset forms of the disease.52, 53
MYOC mutations were initially identified in JOAG. However, the most common MYOC mutation, the Gln368Stop mutation, is also highly associated with the development of late-onset POAG.23 There is no statistically significant difference in the mean age of disease onset between POAG or ocular hypertensive patients who harbor the MYOC Gln368Stop mutation and patients without the mutation.54
On the basis of the age of onset for glaucoma, IOP values, and treatment needs, it seems there is a correlation between risk grade and patient’s phenotype. The Gln368Stop mutation confers mild risk,55 Thr377Met and Gly252Arg mutations intermediate risk,56, 57 and the Pro370Leu mutation severe risk.58, 59, 60, 61
MYOC protein and glaucoma pathogenesis
Most ocular tissues produce MYOC, including the TM, sclera, iris, cornea, lens, ciliary body, retina, and the optic nerve, and MYOC protein has also been isolated from vitreous humor.62, 63, 64, 65
In the TM, MYOC associates with intracellular vesicles, but it is also found in the extracellular space. Hardy et al66 suggested that both native and recombinant MYOC are associated with an extracellular membrane population having biochemical characteristics of exosomes (multivesicular bodies releasing their luminal contents into the extracellular compartment) and containing the major histocompatibility complex class II antigen, HLA-DR. According to their suggestions, MYOC-associated exosomes function in the initiation of ocular immune responses and that may have a role in the regulation of IOP in the normal and glaucomatous human eye.
The most prevalent hypothesis for how MYOC mutations lead to POAG is that mutant MYOC interferes with protein trafficking. The formation of intracellular misfolded MYOC protein leads to decreased outflow by a mechanism that is yet not clear, and this in turn affects IOP regulation.23
Sohn et al67 investigated whether MYOC induction can lead to IOP elevation or vice versa and if any MYOC promoter variant is associated with POAG. Their results do not support the hypothesis that MYOC induction might be linked to IOP variation and that promoter variants of MYOC could be a risk factor for the pathogenesis of POAG. Fingert et al68 had previously shown that variations in the MYOC coding sequences or proximal promoter do not appear to be involved in the development of steroid-induced glaucoma. Jacobson et al69 showed that normal MYOC was secreted from cultured ocular (TM) cells, but very little to no MYOC was secreted from cells expressing five different mutant forms of MYOC. Additionally, no mutant MYOC was detected in the aqueous humor of patients harboring a nonsense MYOC mutation.69 Such data excludes the possibility of MYOC mutant protein having a direct and simple link to POAG. The pathophysiology of MYOC glaucoma is still unclear.
However, there is no doubt that the discovery of the first gene associated with glaucoma was a most important breakthrough in the investigation of the role of inheritance in glaucoma. The following recent findings constitute an attempt to explain how MYOC mutations can lead to IOP elevation and to the development of POAG.
MYOC is expressed in multiple ocular tissues as mentioned above, but its interaction with the mitochondria in the TM and in astrocytes appears to be cell specific.70, 71 On the basis of this finding, He et al72 reported that TM cells overexpressing Pro370Leu mutant MYOC demonstrate features of mitochondrial dysfunction and, thus, Pro370Leu mutant MYOC may increase vulnerability of TM cells to cellular insults and cause impaired function and even cell death. The investigators above showed that MYOC causes disregulation of calcium channels causing mitochondrial membrane depolarization in TM cells, TM contraction, and subsequently leading to reduced outflow and IOP elevation. Pro370Leu mutant MYOC further decreases mitochondrial membrane potential in TM cells. Therefore, they suggested preventive measures targeting mitochondrial protection to delay the onset of the disease in patients carrying the specific MYOC mutation.
Another investigation correlating POAG development with MYOC mutations relates to the effects of wild-type and mutant MYOC, as well as of OPTN on neurite outgrowth in neuronal cells. Koga et al73 demonstrated that overexpression of wild-type MYOC or P370L and Q368X mutants, but not OPTN, caused an inhibition of neurite outgrowth and thus may contribute to the development of neurodegenerative glaucoma.73
OPTN at the GLC1E locus
The second gene associated with POAG was identified in 2002 and it was given the name OPTN (OPTN for optic neuropathy-inducing protein) by Rezaie et al.9
An adult-onset POAG locus had been previously mapped on chromosome 10p14–p15, the GLC1E locus, in a linkage study of a large British family in which 15 of 46 family members were affected with NTG.10 After excluding four genes, Rezaie et al9 selected OPTN as a candidate gene on the basis of its physical location in this region and its expression in retina. They identified a recurrent missense mutation, E50K, segregating in family members who were affected, asymptomatic gene carriers, unaffected, and spouses. 18.4% of the affected subjects had elevated IOP and the remaining had normal IOP up to 21 mm Hg. They suggested that mutations in OPTN may be responsible for 16.7% of the hereditary forms of NTG and that there is an additional risk factor of 13.6% in both familial and sporadic cases. They also demonstrated further expression of OPTN in human TM, non-pigmented ciliary epithelium, retina, brain, adrenal cortex, liver, fetus, lymphocyte, and fibroblast.
However, no other subsequent report showed such a high prevalence of mutations in OPTN to be responsible for hereditary forms of NTG. Also, the only mutation in OPTN, that was strongly associated with NTG, was the E50K change. The prevalence of E50K may finally be <2% in NTG patients and <1% in POAG overall.74, 75, 76
OPTN and glaucoma pathogenesis
The OPTN gene had been first identified as FIP2. Tumor necrosis factor-α (TNF-α) is a proinflammatory cytokine, which has a number of important biological functions, and one of them is to control viral infection.77 In an attempt to understand the mechanism by which the viral proteins inhibit TNF-α functions, Yongan Li et al78 identified a gene, FIP-2 (for 14.7K-interacting protein), interacting with E3-14.7K, a protein that is one of the several inhibitors of TNF-α cytolysis. The investigators found that FIP-2 reverses the protective effect of E3-14.7K on TNF receptor-induced cytolysis. Their study suggested that FIP-2 is a component of the TNF-α signaling pathway. Expression of FIP-2 protein blocks the protective effect of E3-14.7K and it is therefore possible that FIP-2 can utilize some inducible cellular cofactors to activate the cell death pathway.
TNF-α increases the severity of damage in the ONH in both POAG and in NTG patients.79, 80 According to Rezaie et al9, if wild-type OPTN has a neuroprotective role against TNF-α-induced cytolysis, the defective protein can lead to optic neuropathy and visual loss, despite normal IOP in NTG.
De Marco et al81 further explored the role of OPTN in cell survival. After confirming Rezaie's findings regarding localization of OPTN in the Golgi and having accepted OPTN to be directly involved in the survival of RGCs in a cell autonomous manner, they showed that OPTN translocates to the nucleus upon oxidative stress, using a mouse model. This translocation was dependent on the GTPase activity of an interactor of OPTN, Rab8, which is involved in membrane trafficking that promotes changes in cell shape. Although wild-type OPTN is overexpressed to protect cells from oxidative stress-induced apoptosis, the disease-causing E50K OPTN mislocalises, loses its ability to respond to oxidative stress, and its overexpression results in the release of cytochrome c, loss of mitochondrial membrane potential, and activation of the mitochondrial pathway in neuronal cell apoptosis.
On the contrary, Koga et al73 recently showed that overexpression of wild-type OPTN results in increased apoptosis of RGCs and that OPTN (wild type or the E50K mutant form), unlike MYOC, is devoid of effects on neurite outgrowth in neuronal cells. They concluded that MYOC and OPTN appear to have different functions and may contribute to the development of neurodegenerative glaucoma via distinct mechanisms, which are still largely unknown.
The controversial role of WDR36 and NTF4 in POAG
There is great uncertainty among experts about the contribution of WDR36 and NTF4 and their variants in the pathogenesis of glaucoma. Unlike the original reports on the role of WDR36 and NTF4, many others followed, which failed to replicate the original studies in which the above genes were presented as glaucoma-causing genes. The data are currently inconclusive and, before presenting them in this review, it is useful to mention that WDR36 and NTF4 could be classified in a group of controversial genes that do not have an established role in glaucoma pathogenicity at present.
WDR36 at the GLC1G locus
In 2005, Monemi et al46 described mapping of a new locus for POAG at the 5q22.1 region. The locus was named GLC1G and the candidate gene for GLC1G was identified as WDR36. WDR36 is expressed in the lens, iris, sclera, ciliary muscles, ciliary body, TM, retina, and the optic nerve. The investigators above observed WDR36 mutations in subjects with either high-pressure or low-pressure glaucoma and they concluded that WDR36 is involved in both types of glaucoma and IOP. In two of the seven GLC1G-linked families, they did not find any DNA coding variations in the coding regions of the WDR36 gene, and they explained this finding on the basis of mutations in another POAG gene at GLC1G.
The association of POAG with WDR36 does not replicate in all populations from the United States,82, 83 Canada,84 Australia,85 and Germany.86 In all these reports, WDR36 variants, including the D658G variant, which was used by Monemi to assert that WDR36 is a glaucoma gene, were equally found in patients and controls and failed to segregate with POAG. There are families linked to the GLC1G locus in which a WDR36 mutation cannot be detected.87, 88, 89
WDR36 and POAG pathogenesis
In terms of neuroprotection as a complimentary treatment in glaucoma, Bakalash et al90 vaccinated experimental animals with an agent that suppresses human autoimmune disease and alters immune function by engaging the T-cell receptor. They found that vaccination with this agent can protect RGCs from the consequences of elevated IOP in rats.90 Therefore, T-cell-mediated responses may participate in glaucoma-associated optic neuropathy. On the basis of the use of DNA microarrays, Mao et al91 had previously looked for genes specifically involved in human T-cell activation, and one of them was WDR36, which highly co-regulated with interleukin-2.
Monemi et al46 observed that one of the four identified disease-causing mutations of WDR36, D658G, maps to the C-terminal part of the cytochrome heme cd1 domain, which is part of an enzyme with cytochrome oxidase activity. A gene responsible for primary congenital glaucoma, cytochrome P450, subfamily 1, polypeptide 1 (CYP1B1), is also a member of the cytochrome P450 family. Thus, they suggested a functional association between the two genes.46
Skarie and Link92 showed that at the cellular level, loss of Wdr36 disrupts ribosomal RNA maturation and leads to nucleolar morphology defects, resulting in activation of the p53 stress–response pathway. In POAG, it is established that RGCs are lost because of apoptosis93, 94 and p53 is a key regulator of the apoptotic pathway. Their data showing an interaction of p53 and WDR36 suggest that variants in these genes could potentially synergize in POAG pathogenesis.
The NTF4 gene and POAG
Wiggs et al15 perfomed a two-stage genome-wide scan to identify the genomic locations of adult-onset glaucoma susceptibility genes. They identified several potential loci, including regions on chromosomes 2, 14, 17, and 19. Subsequently, at the chromosome 19 locus, Pasutto et al47 reported seven different heterozygous mutations in the NTF4 gene. This accounted for about 1.7% of POAG patients of European origin. Vithana et al48 also identified a single mutation in the NTF4 gene accounting for <1% of POAG patients in a Chinese population. Liu et al95 recently reported that coding variants in the NTF4 gene were not associated with an elevated risk of POAG in a United States Caucasian population. There were phenotypic differences between the study populations such as differences in the mean age, in the subtypes of glaucoma, as well as ethnic differences that could explain the discrepant findings. However, a similar investigation in an Indian population also did not replicate an association of variations in the NTF4 gene with POAG.96
NT-4 normally activates tyrosine kinase-B receptor (TrkB) present in the RGCs and therefore is considered to play a protective role against high IOP, ischemia and release of cytotoxins.97, 98, 99, 100, 101 According to Pasutto et al47, mutations in the NTF4 gene resulted in the impairment of TrkB signaling, as well as neuronal growth, and therefore, the NTF4 variants may have a significant effect on neuronal survival. They postulated that agents activating TrkB could therefore be a novel glaucoma treatment.47 However, Rohrer et al102 recently examined the roles of TrkB receptor isoforms in early postnatal survival in wild-type and mutant mice lacking all isoforms of TrkB. They found that TrkB signaling is not required for survival of RGCs during the period of target-dependent survival, but does appear to reduce degeneration of RGCs in adult animals.102
Other loci, genes, and low-penetrance risk alleles associated with POAG
Fuse22 presented a list of 27 POAG and NTG genes that have been identified from association studies between 2005 and 2010. Among them, apolipoprotein E (APOE) at 19q13.2,103 TNF at 6p21.3,104 the toll-like receptor 4 (TLR4) gene at 9q32–q33,105 optic atrophy 1 (OPA1) gene at 3q28–q29,106 and tumor protein p53 (TP53) at 17p13.1.107 CYP1B1 at 2p22-p21 has been associated with JOAG first by Vincent et al108 and later by other investigators as well.109
Fingert et al110 recently mapped a new NTG gene to chromosome 12q14, the TANK-binding kinase-1 (TBK1). CNVs that encompass the TBK1 gene were associated with the development of NTG.
Another recent GWAS conducted in Japan by Meguro et al111 showed that common variants in the S1 RNA-binding domain 1 (SRBD1) and elongation of long-chain fatty acids family member 5 (ELOVL5) genes contribute to NTG susceptibility.
Secreted protein acidic and rich in cysteine (SPARC) is a matricellular glycoprotein, which promotes extracellular matrix deposition.112 It distributes throughout the TM and it has been considered to have an important role in IOP regulation.113 SPARC has also been detected in the iris of POAG patients,114 while Seet et al115 have found that SPARC deficiency in mice resulted in improved surgical survival in a mouse model of glaucoma filtration surgery. Aroca-Aguilar et al116 reported an interaction between recombinant MYOC and SPARC. They suggested that proteolytic processing of MYOC modulates this interaction.116 Chen et al117 recently evaluated the involvement of SPARC mutations and CNVs in JOAG. The same group had previously located the gene at chromosome 5q in a region within the GLCM1 locus.88 They finally excluded SPARC as the causal gene at the GLCM1 locus by revealing that coding sequences, splice sites, and copy number of SPARC do not contribute to JOAG. According to the investigators, further studies are required to unravel the involvement of SPARC in the pathogenesis of glaucoma and the causal gene for GLCM1 locus remains unidentified.117
Thorleifsson et al28 conducted a genome-wide association study for POAG to search for genomic variants that confer risk of POAG in an Icelandic population of 1263 patients and 34877 controls. After testing 303117 SNPs for association with POAG, they found one, rs4236601[A] at 7q31, located close to CAV1 and CAV2 (encoding caveolin1 and 2) to be associated with POAG. The association was investigated in POAG cases and controls from Sweden, Leicester and Southampton in the UK, as well as from Australia. CAV1 and 2 are involved in the formation of invaginations of the plasma membrane called caveolae and both are expressed in TM and RGCs of the eye.118, 119 Their role in signal transduction has been already studied and an interaction of CAV1 and endothelial nitric oxide synthase, which leads to inactivation of the latter and therefore reduces nitric oxide production, has been established.120, 121 Nitric oxide overproduction causes cytotoxicity, neurodegeneration, cell apoptosis, and circulatory failure. CAV1 is also a regulator of transforming growth factor-β (TGF-β) type 1 receptor.122 Both nitric oxide and TGF-β are implicated in the pathogenesis of POAG.123, 124 Although no direct correlation of the above POAG variant and CAV1 or CAV2 expression was observed, Thorleifsson et al28 concluded that the effect of rs4236601 on CAV1 and CAV2 expression in ocular tissue can not be excluded. However, this association was not replicated in the UK cohorts (P>0.05), as well as by Fingert et al125 in an Iowa population.
Burdon et al126 recently reported a GWAS in Australians of European descent, which identified two susceptibility loci for advanced POAG at TMCO1 (encoding a transmembrane protein with a coiled-coil domain) and CDKN2B-AS1 (cyclin-dependent kinase inhibitor 2B), imparting a threefold increase in risk for carriers of one or more risk alleles at the two loci. A role for both TMCO1 and CDKN2B-AS1 in the retinal ganglion cell apoptosis was proposed.126
The most recently published study regarding identification of new loci associated with POAG is the one by Porter et al127 who identified a new POAG locus, GLC1Q, on chromosome 4 at 4q35.1–q35.2. They investigated the genetic cause of POAG in a large four-generation family with an apparent autosomal dominant mode of inheritance using genome-wide linkage analysis, but they failed to identify a mutation within the critical region in the candidate genes LRPB2BP, CYP4V2 and UFSP2.127
Table 1 presents the most common and most recently found genes associated with POAG, data on relevant original and replication reports, as well as the reported prevalence of each gene mutation in POAG populations.
The role of endophenotypes in glaucoma
‘Endophenotypes’ is a psychiatric concept described as internal phenotypes discoverable by a ‘biochemical test or microscopic examination’.128, 129 An endophenotype-based approach has the potential to assist in the genetic dissection of complex diseases. Endophenotypes are a special kind of biomarker, as long as they fulfill the criteria suggested. The endophenotype must be associated with disease in the population, it has to be heritable, it must be primarily state-independent (manifests in an individual whether or not illness is active), endophenotype and illness have to co-segregate within families, and finally, the endophenotype found in affected family members has to be found in non-affected family members at a higher rate than in the general population.130, 131
Quantitative traits refer to phenotypes that vary in degree and represent the product of polygenic effects. Mapping genes influencing the related quantitative trait, rather than the complete complex phenotype, has several important advantages, including objective phenotype definitions and a possible reduction in the underlying molecular heterogeneity.132
It has been already stated that complex disorders such as glaucoma result from the combined interaction of genes and environmental factors, and that several risk factors have been evaluated for POAG. Among the established risk factors for POAG, IOP, optic nerve cupping as measured by vertical cup-to-disc ratio, and central corneal thickness (CCT) represent plausible endophenotypes.133, 134, 135 In the Beaver Dam Eye Study, IOP, optic cup diameter, optic disc diameter, and cup-to-disc ratio were estimated to have heritability estimates of 0.36, 0.55, 0.57, and 0.48, respectively.136 In the Glaucoma Inheritance Study in Tasmania, visual field defect, IOP and, optic disc cupping were ranked in an attempt to predict whether a person in a glaucoma pedigree would develop glaucoma, even at an early stage.137
In the context of establishing a genetic correlation between POAG endophenotypes and POAG, a genome-wide scan of IOP was performed, using 486 pedigrees ascertained through a population-based cohort, the Beaver Dam Eye Study.138 The investigators’ purpose was to identify quantitative trait loci controlling IOP and thereby influencing the development of glaucoma. Seven loci of interest were identified (2, 5, 6, 7, 12, 15, and 19) and two of the regions (on chromosomes 2 and 19) co-localized with blood pressure loci. The authors concluded that understanding the mechanism of elevated IOP may help elucidate the understanding of both hypertension and glaucoma.
CCT is a risk factor of glaucoma. Vithana et al139 conducted two GWAS for CCT in 5080 individuals drawn from two ethnic populations in Singapore (Indian and Malays) and identified novel genetic loci significantly associated with CCT (COL8A2 rs96067 and interval of RXRA-COL5A1 rs1536478). They confirmed the involvement of a previously reported gene for CCT and brittle cornea syndrome (ZNF469 rs9938149 and rs12447690), and they showed an association exceeding the formal threshold for genome-wide significance of COL5A1 rs7044529 and CCT. Their findings implicate the involvement of collagen genes influencing CCT and thus, possibly the pathogenesis of glaucoma.139
Khor et al140 conducted a GWAS on 4445 Singaporean individuals with replication in Rotterdam, the Netherlands, on 9326 individuals of Caucasian ancestry, using the most widely reported parameter for optic disc traits, the optic disc area. They identified a novel locus on chromosome 22q13.1, CARD10, which strongly associates with optic disc area in both Singaporean cohorts as well as in the Rotterdam Study, and confirmed the association between CDC7/TGFBR3 and ATOH7 and the optic disc area in Asians, suggesting that there are general genetic determinants applicable to the size of the optic disc across different ethnicities.140
The results of quantitative trait analysis can complement the findings from GWAS; for example, Rotimi et al87 in 2006 suggested a locus on 5q22 was linked to high IOP and this lies within the WDR36 gene, which is implicated in POAG.
Therapeutic implications of genetics for POAG
RGC death is the final outcome of all pathogenetic mechanisms causing POAG. The putative mechanisms of how this occurs are legion. They include pressure-induced injury of the ONH, leading to retinal gene expression alterations,44, 141 astrocyte response to changes in IOP,142 oxidative stress, mitochondrial dysfunction, neurotrophic factors,143, 144 and autoimmunity.145 Identifying validated genetic mutations that are replicated in multiple populations perhaps offers the best hope of correct identification of the most important pathways, which result in RGC death. This in turn should identify novel treatment strategies.
For example, Li et al146 recently proposed RNA interference (RNAi) as a gene silencing therapy for complete elimination of mutant MYOC from human TM cells.146 Using RNAi,147, 148, 149, 150 they eliminated mutant MYOC in HTM cells. Mutant MYOC is insufficiently folded and accumulates in the ER,151, 152 causing the unfolded protein response with subsequently activated cell apoptosis.
An important goal of genetic studies in glaucoma is the development of personalized medicine for patients. If sufficient specificity and sensitivity can be generated, then patients could be genotyped before symptomatic vision loss has occurred and either begin preventative treatment or be discharged.
Allingham et al23 suggested genetic screening would provide focused delivery of medical resources on smaller at-risk populations if risk assessment reaches a sufficient threshold of accuracy.
Ennis et al153 conducted MYOC glaucoma screening in a regional glaucoma service in southern England, to identify the prevalence of MYOC gene mutations in a UK glaucoma cohort. They suggested that by identifying first-degree relatives without MYOC mutations, these patients might be released from traditional intensive screening programs.
Comments: future genetic approaches
POAG is a complex, heterogenous disease for which the genetic contribution still needs to be identified in over 95% of the cases. POAG is also a common disease in terms of prevalance and distribution in various populations. However, its prevalence varies in different racial/ethnic populations; for example, there is higher prevalance of POAG in African Americans than in Americans of European ancestry. It is unknown whether genetic factors are responsible for this difference.154 There are also gene mutations associated with POAG, which are not common in all populations.50
New approaches may help identify these as yet unidentified genetic variations. One approach to the whole genome association mapping that exploits linkage disequilibrium generated by admixture between genetically distinct ancestral populations is called ‘admixture mapping’,155 and can be an interesting and practical genetic approach in POAG. Although GWAS are more powerful compared with linkage analysis to discover genes of weak effect that might contribute to the development of POAG, they can be extremely expensive as they require the use of thousands of markers to locate genes associated with the disease. Admixture mapping requires considerably fewer markers and is considered to be more robust to allelic heterogeneity.155, 156
To overcome the missing genetic control due to gene variants that are too rare to be picked up by GWAS, ‘next-generation sequencing technologies’ could also rapidly facilitate substantial progress.157
In conclusion, identification of genetic determinants of POAG is still a work in progress. New genetic sequencing technologies, increased cohort sizes, and detailed phenotyping will undoubtedly identify novel genetic variants. The association of complement gene mutations in AMD has led to the development of novel therapies for AMD. It is expected that identifying novel genetic variants in POAG will also result in novel treatment paradigms. Thus, ongoing studies are worth pursuing.
References
Quigley HA . Number of people with glaucoma worldwide. Br J Ophthalmol 1996; 80: 389–393.
Kumar A, Basavaraj MG, Gupta SK, Qamar I, Ali AM, Bajaj V et al. Role of CYP1B1, MYOC, OPTN and OPTC genes in adult-onset primary open-angle glaucoma: predominance of CYP1B1 mutations in Indian patients. Mol Vis 2007; 13: 667–676.
Werner EB . Normal tension glaucoma. In: Ritch R, Shields MB, Krupin T (eds). The Glaucomas, 2nd ed. Mosby: St Louis, 1996, pp 769–797.
Wilson MR, Hertzmark E, Walker AM, Childs-Shaw K, Epstein DL . A case-control study of risk factors in open angle glaucoma. Arch Ophthalmol 1987; 105: 1066–1071.
Tielsch JM, Katz J, Sommer A, Quigley HA, Javitt JC . Family history and risk of primary open angle glaucoma. The Baltimore Eye Survey. Arch Ophthalmol 1994; 112: 69–73.
Fan BJ, Leung YF, Wang N, Lam SC, Liu Y, Tam OS et al. Genetic and environmental risk factors for primary open angle glaucoma. Chin Med J 2004; 117: 706–710.
Fingert JH, Stone EM, Sheffield VC, Alward WL . Myocilin glaucoma. Surv Ophthalmol 2002; 47: 547–561.
Nemesure B, Jiao X, He Q, Leske MC, Wu SY, Hennis A et al. A genome-wide scan for primary open-angle glaucoma (POAG): the Barbados Family Study of Open-Angle Glaucoma. Hum Genet 2003; 112: 600–609.
Rezaie T, Child A, Hitchings R, Brice G, Miller L, Coca-Prados M et al. Adult-onset primary open-angle glaucoma caused by mutations in optineurin. Science 2002; 295: 1077–1079.
Sarfarazi M, Child A, Stoilova D, Brice G, Desai T, Trifan OC et al. Localization of the fourth locus (GLC1E) for adult-onset primary open-angle glaucoma to the 10p15-p14 region. Am J Hum Genet 1998; 62: 641–652.
Sheffield VC, Stone EM, Alward WL, Drack AV, Johnson AT, Streb LM et al. Genetic linkage of familial open angle glaucoma to chromosome 1q21-q31. Nat Genet 1993; 4: 47–50.
Stoilova D, Child A, Trifan OC, Crick RP, Coakes RL, Sarfarazi M . Localization of a locus (GLC1B) for adult-onset primary open angle glaucoma to the 2cen-q13 region. Genomics 1996; 36: 142–150.
Stone EM, Fingert JH, Alward WL, Nguyen TD, Polansky JR, Sunden SL et al. Identification of a gene that causes primary open angle glaucoma. Science 1997; 275: 668–670.
Trifan OC, Traboulsi EI, Stoilova D, Alozie I, Nguyen R, Raja S et al. A third locus (GLC1D) for adult-onset primary open-angle glaucoma maps to the 8q23 region. Am J Ophthalmol 1998; 126: 17–28.
Wiggs JL, Allingham RR, Hossain A, Kern J, Auguste J, DelBono EA et al. Genome-wide scan for adult onset primary open angle glaucoma. Hum Mol Genet 2000; 9: 1109–1117.
Wirtz MK, Samples JR, Kramer PL, Rust K, Topinka JR, Yount J et al. Mapping a gene for adult-onset primary open-angle glaucoma to chromosome 3q. Am J Hum Genet 1997; 60: 296–304.
Wirtz MK, Samples JR, Rust K, Lie J, Nordling L, Schilling K et al. GLC1F, a new primary open-angle glaucoma locus, maps to 7q35-q36. Arch Ophthalmol 1999; 117: 237–241.
Wolfs RC, Klaver CC, Ramrattan RS, van Duijn CM, Hofman A, de Jong PT . Genetic risk of primary open angle glaucoma. Population based familial aggregation study. Arch Ophthalmol 1998; 116: 1640–1645.
Strachan T, Read A . Human Molecular Genetics, 3rd ed. Garland Science: New York, 2004, pp 102–119.
Lander ES, Schork NJ . Genetic dissection of complex traits. Science 1994; 265: 2037–2048.
Rieger R, Michaelis A, Green MM . Glossary of Genetics: Classical and Molecular, 5th ed. Dictionary of Modern Medicine Segen, 1992.
Fuse N . Genetic basies for glaucoma. Tohoku J Exp Med 2010; 221: 1–10.
Allingham RR, Liu Y, Rhee DJ . The genetics of primary open-angle glaucoma: a review. Exp Eye Res 2009; 88: 837–844.
Feero WG, Guttmacher AE, Collins FS . The genome gets personal–almost. JAMA 2008; 299: 1351–1352.
Easton DF, Pooley KA, Dunning AM, Pharoah PD, Thompson D, Ballinger DG et al. Genome-wide association study identifies novel breast cancer susceptibility loci. Nature 2007; 447: 1087–1093.
Zanke BW, Greenwood CM, Rangrej J, Kustra R, Tenesa A, Farrington SM et al. Genome-wide association scan identifies a colorectal cancer susceptibility locus on chromosome 8q24. Nat Genet 2007; 39: 989–994.
Mathew CG . New links to the pathogenesis of Crohn disease provided by genome-wide association scans. Nat Rev Genet 2008; 9: 9–14.
Thorleifsson G, Walters GB, Hewitt AW, Masson G, Helgason A, DeWan A et al. Common variants near CAV1and CAV2 are associated with primary open angle glaucoma. Nat Genet 2010; 42: 906–910.
Nakanoa M, Ikeda Y, Taniguchia T, Yagi T, Fuwa M, Omi N et al. Three susceptible loci associated with primary open-angle glaucoma identified by genome-wide association study in a Japanese population. Proc Natl Acad Sci USA 2009; 106: 12838–12842.
Iafrate AJ, Feuk L, Rivera MN, Listewnik ML, Donahoe PK, Qi Y et al. Detection of large-scale variation in the human genome. Nat Genet 2004; 36: 949–951.
Sebat J, Lakshmi B, Troge J, Alexander J, Young J, Lundin P et al. Large-scale copy number polymorphism in the human genome. Science 2004; 305: 525–528.
Sharp AJ, Locke DP, McGrath SD, Cheng Z, Bailey JA, Vallente RU et al. Segmental duplications and copy-number variation in the human genome. Am J Hum Genet 2005; 77: 78–88.
Tuzun E, Sharp AJ, Bailey JA, Kaul R, Morrison VA, Pertz LM et al. Fine- scale structural variation of the human genome. Nat Genet 2005; 37: 727–732.
Conrad DF, Andrews TD, Carter NP, Hurles ME, Pritchard JK . A high-resolution survey of deletion polymorphism in the human genome. Nat Genet 2006; 38: 75–81.
Hinds DA, Kloek AP, Jen M, Chen X, Frazer KA . Common deletions and SNPs are in linkage disequilibrium in the human genome. Nat Genet 2006; 38: 82–85.
McCarroll SA, Hadnott TN, Perry GH, Sabeti PC, Zody MC, Barrett JC et al. Common deletion polymorphisms in the human genome. Nat Genet 2006; 38: 86–92.
Locke DP, Sharp AJ, McCarroll SA, McGrath SD, Newman TL, Cheng Z et al. Linkage disequilibrium and heritability of CNPs within duplicated regions of the human genome. Am J Hum Genet 2006; 79: 275–290.
Redon R, Ishikawa S, Fitch KR, Feuk L, Perry GH, Andrews TD et al. Global variation in copy number in the human genome. Nature 2006; 444: 444–454.
Feinberg AP . Phenotypic plasticity and the epigenetics of human disease. Nature 2007; 447: 433–440.
McCarroll SA, Altshuler DM . Copy-number variation and association studies of human disease. Nat Genet 2007; 39: S37–S42.
Davis LK, Meyer KJ, Schindler EI, Beck J, Rudd D, Grundstad AJ et al. Copy number variations (CNVs) and primary open angle glaucoma (POAG). Invest Ophthalmol Vis Sci 2011; 52: 7122–7133.
Schena M . Genome analysis with gene expression microarrays. Bioessays 1996; 18: 427–431.
Leung YF, Tam PO, Lee WS, Lam DS, Yam HF, Fan BJ et al. The dual role of dexamethazone on anti- inflammation and outflow resistance demonstrated in cultured human trabecular meshwork cells. Mol Vis 2003; 9: 425–439.
Johnson EC, Jia L, Cepurna WO, Doser TA, Morrison JC . Global changes in optic nerve head gene expression after exposure to elevated intraocular pressure in a rat glaucoma model. Invest Ophthalmol Vis Sci 2007; 48: 3161–3177.
Fan BJ, Wang DY, Lam DS, Pang CP . Gene mapping for primary open angle glaucoma. Clin Biochem 2006; 39: 249–258.
Monemi S, Spaeth G, DaSilva A, Popinchalk S, Ilitchev E, Liebmann J et al. Identification of a novel adult-onset primary open-angle glaucoma (POAG) gene on 5q22.1. Hum Mol Genet 2005; 14: 725–733.
Pasutto F, Matsumoto T, Mardin CY, Sticht H, Brandstätter JH, Michels-Rautenstrauss K et al. Heterozygous NTF4 mutations impairing neurotrophin-4 signaling in patients with primary open-angle glaucoma. Am J Hum Genet 2009; 85: 447–456.
Vithana EN, Nongpiur ME, Venkataraman D, Chan SH, Mavinahalli J, Aung T . Identification of a novel mutation in the NTF4 gene that causes primary open-angle glaucoma in a Chinese population. Mol Vis 2010; 16: 1640–1645.
Morissette J, Cote G, Anctil JL, Plante M, Amyot M, Héon E et al. A common gene for juvenile and adult-onset primary open-angle glaucomas confined on chromosome 1q. Am J Hum Genet 1995; 56: 1431–1432.
Gong G, Kosoko-Lasaki O, Haynatzki GR, Wilson MR . Genetic dissection of myocilin glaucoma. Hum Mol Genet 2004; 13: 91–102.
Fingert JH, Héon E, Liebmann JM, Yamamoto T, Craig JE, Rait J et al. Analysis of myocilin mutations in 1703 glaucoma patients from five different populations. Hum Mol Genet 1999; 8: 899–905.
Alward WL, Fingert JH, Coote MA, Johnson AT, Lerner SF, Junqua D et al. Clinical features associated with mutations in the chromosome 1 open-angle glaucoma gene (GLC1A). N Engl J Med 1998; 338: 1022–1027.
Hewitt AW, Bennett SL, Fingert JH, Cooper RL, Stone EM, Craig JE et al. The optic nerve head in myocilin glaucoma. Invest Ophthalmol Vis Sci 2007; 48: 238–243.
Graul TA, Kwon YH, Zimmerman MB, Kim CS, Sheffield VC, Stone EM et al. A case-control comparison of the clinical characteristics of glaucoma and ocular hypertensive patients with and without the myocilin Gln368Stop mutation. Am J Ophthalmol 2002; 134: 884–890.
Craig JE, Baird PN, Healey DL, McNaught AI, McCartney PJ, Rait JL et al. Evidence for genetic heterogeneity within eight glaucoma families, with the GLC1A Gln368STOP mutation being an important phenotypic modifier. Ophthalmology 2001; 108: 1607–1620.
Mackey DA, Healey DL, Fingert JH, Coote MA, Wong TL, Wilkinson CH et al. Glaucoma phenotype in pedigrees with the myocilin Thr377Met mutation. Arch Ophthalmol 2003; 121: 1172–1180.
Hewitt AW, Bennett SL, Richards JE, Dimasi DP, Booth AP, Inglehearn C et al. Myocilin Gly252Arg mutation and glaucoma of intermediate severity in Caucasian individuals. Arch Ophthalmol 2007; 125: 98–104.
Adam MF, Belmouden A, Binisti P, Brézin AP, Valtot F, Béchetoille A et al. Recurrent mutations in a single exon encoding the evolutionarily conserved olfactomedin homology domain of TIGR in familial open-angle glaucoma. Hum Mol Genet 1997; 6: 2091–2097.
Rozsa FW, Shimizu S, Lichter PR, Johnson AT, Othman MI, Scott K et al. GLC1A mutations point to regions of potential functional importance on the TIGR/MYOC protein. Mol Vis 1998; 4: 20.
Ge J, Zhuo Y, Guo Y, Ming W, Yin W . Gene mutation in patients with primary open-angle glaucoma in a pedigree in China. Chin Med J (Engl) 2000; 113: 195–197.
Wei YT, Duan S, Ge J, Zhuo YH, Ling YL, Lin MK et al. A preliminary Study on gene mutation and its function in a large family (GZ.1 pedigree) with open-angle glaucoma]. Zhonghua Yan Ke Za Zhi 2005; 41: 1068–1075.
Karali A, Russell P, Stefani FH, Tamm ER . Localization of myocilin/trabecular meshwork—inducible glucocorticoid response protein in the human eye. Invest Ophthalmol Vis Sci 2000; 41: 729–740.
Kubota R, Noda S, Wang Y, Minoshima S, Asakawa S, Kudoh J et al. A novel myosin-like protein (myocilin) expressed in the connecting cilium of the photoreceptor: molecular cloning, tissue expression, and chromosomal mapping. Genomics 1997; 41: 360–369.
Ortego J, Escribano J, Coca-Prados M . Cloning and characterization of subtracted cDNAs from a human ciliary body library encoding TIGR, a protein involved in juvenile open angle glaucoma with homology to myosin and olfactomedin. FEBS Lett 1997; 413: 349–353.
Swiderski RE, Ross JL, Fingert JH, Clark AF, Alward WL, Stone EM et al. Localization of MYOC transcripts in human eye and optic nerve by in situ hybridization. Invest Ophthalmol Vis Sci 2000; 41: 3420–3428.
Hardy KM, Hoffman EA, Gonzalez P, McKay BS, Stamer WD . Extracellular trafficking of myocilin in human trabecular meshwork cells. J Biol Chem 2005; 280: 28917–28926.
Sohn S, Hur W, Choi YR, Chung YS, Ki CS, Kee C . Little evidence for association of the glaucoma gene MYOC with open-angle glaucoma. Br J Ophthalmol 2010; 94: 639–642.
Fingert JH, Clark AF, Craig JE, Alward WL, Snibson GR, McLaughlin M et al. Evaluation of the myocilin (MYOC) glaucoma gene in monkey and human steroid-induced ocular hypertension. Invest Ophthalmol Vis Sci 2001; 42: 145–152.
Jacobson N, Andrews M, Shepard AR, Nishimura D, Searby C, Fingert JH et al. Non-secretion of mutant proteins of the glaucoma gene myocilin in cultured trabecular meshwork cells and in aqueous humor. Hum Mol Genet 2001; 10: 117–125.
Wentz-Hunter K, Ueda J, Shimizu N, Yue BY . Myocilin is associated with mitochondria in human trabecular meshwork cells. J Cell Physiol 2002; 190: 46–53.
Wentz-Hunter K, Shen X, Yue BY . Distribution of myocilin, a glaucoma gene product, in human corneal fibroblasts. Mol Vis 2003; 9: 308–314.
He Y, Leung KW, Zhuo YH, Ge J . Pro370Leu mutant myocilin impairs mitochondrial functions in human trabecular meshwork cells. Mol Vis 2009; 15: 815–825.
Koga T, Shen X, Park J-S, Qiu Y, Park BC, Shyam R et al. Differential effects of myocilin and optineurin, two glaucoma genes, on neurite outgrowth. Am J Pathol 2010; 176: 343–352.
Alward WL, Kwon YH, Kawase K, Craig JE, Hayreh SS, Johnson AT et al. Evaluation of optineurin sequence variations in 1048 patients with open-angle glaucoma. Am J Ophthalmol 2003; 136: 904–910.
Aung T, Ebenezer ND, Brice G, Child AH, Prescott Q, Lehmann OJ et al. Prevalence of optineurin sequence variants in adult primary open angle glaucoma: implications for diagnostic testing. J Med Genet 2003; 40: e101.
McDonald KK, Abramson K, Beltran MA, Ramirez MG, Alvarez M, Ventura A et al. Myocilin and optineurin coding variants in Hispanics of Mexican descent with POAG. J Hum Genet 2010; 55: 697–700.
Wong GHW, Kamb A, Goeddel DV . Antiviral properties of TNF. In: Beutler B (ed). Tumor Necrosis Factors: the Molecules and Their Emerging Role in Medicine. Raven Press: New York, NY, 1992, pp 371–381.
Li Y, Kang J, Horwitz MS . Interaction of an adenovirus E3 14.7-kilodalton protein with a novel tumor necrosis factor alpha-inducible cellular protein containing leucine zipper domains. Mol Cell Biol 1998; 18: 1601–1610.
Yuan L, Neufeld AH . Tumor necrosis factor-alpha: a potentially neurodestructive cytokine produced by glia in the human glaucomatous optic nerve head. Glia 2000; 32: 42–50.
Tezel G, Wax MB . Increased production of tumor necrosis factor-alpha by glial cells exposed to simulated ischemia or elevated hydrostatic pressure induces apoptosis in cocultured retinal ganglion cells. J Neurosci 2000; 20: 8693–8700.
DeMarco N, Buono M, Troise F, Diez-Roux G . Optineurin increases cell survival and translocates to the nucleus in a Rab8-dependent manner upon an apoptotic stimulus. J Biol Chem 2006; 281: 16147–16156.
Hauser MA, Allingham RR, Linkroum K, Wang J, LaRocque-Abramson K, Figueiredo D et al. Distribution of WDR36 DNA sequence variants in patients with primary open angle glaucoma. Invest Ophthalmol Vis Sci 2006; 47: 2542–2546.
Fingert JH, Alward WL, Kwon YH, Shankar SP, Andorf JL, Mackey DA et al. No association between variations in the WDR36 gene and primary open-angle glaucoma. Arch Ophthalmol 2007; 125: 434–436.
Raymond V, Dubois S, Marquis A, Arseneault R, Duchesne A, Rodrigue M-A . Large scale mutation analysis of the third glaucoma-causing gene, WDR36, at GLC1G in the French-Canadian population of Québec. Presented at the American Society of Human Genetics (ASHG) 55th Annual Meeting; Salt Lake City, UT. Bethesda, MD: ASHG, 2005, p 358.
Hewitt AW, Dimasi DP, Mackey DA, Craig JE . A Glaucoma case control Study of the WDR36 gene D658G sequence variant. Am J Ophthalmol 2006; 142: 324–325.
Pasutto F, Mardin CY, Michels-Rautenstrauss K, Weber BH, Sticht H, Chavarria-Soley G et al. Profiling of WDR36 missense variants in german patients with glaucoma. Invest Ophthalmol Vis Sci 2008; 49: 270–274.
Rotimi CN, Chen G, Adeyemo AA, Jones LS, Agyenim-Boateng K, Eghan Jr BA et al. Genome-wide scan and fine mapping of quantitative trait loci for intraocular pressure on 5q and 14q in West Africans. Invest Ophthalmol Vis Sci 2006; 47: 3262–3267.
Pang CP, Fan BJ, Canlas O, Wang DY, Dubois S, Tam PO et al. A genome-wide scan maps a novel juvenile-onset primary open angle glaucoma locus to chromosome 5q. Mol Vis 2006; 12: 85–92.
Kramer PL, Samples JR, Monemi S, Sykes R, Sarfarazi M, Wirtz MK . The role of the WDR36 gene on chromosome 5q22.1 in a large family with primary open-angle glaucoma mapped to this region. Arch Ophthalmol 2006; 124: 1328–1331.
Bakalash S, Shlomo GB, Aloni E, Shaked I, Wheeler L, Ofri R et al. T-cell-based vaccination for morphological and functional neuroprotection in a rat model of chronically elevated intraocular pressure. J Mol Med 2005; 83: 904–916.
Mao M, Biery MC, Kobayashi SV, Ward T, Schimmack G, Burchard J et al. T-lymphocyte activation gene identification by coregulated expression on DNA microarrays. Genomics 2004; 83: 989–999.
Skarie JM, Link BA . The Primary open-angle glaucoma gene WDR36 functions in ribosomal RNA processing and interacts with the p53 stress–response pathway. Hum Mol Genet 2008; 17 (16): 2474–2485.
Kerrigan LA, Zack DJ, Quigley HA, Smith SD, Pease ME . TUNEL-Positive ganglion cells in human primary open-angle glaucoma. Arch Ophthalmol 1997; 115: 1031–1035.
Nickells RW . Ganglion cell death in glaucoma: from mice to men. Vet Ophthalmol 2007; 10 (Suppl 1): 88–94.
Liu Y, Liu W, Crooks K, Schmidt S, Allingham RR, Hauser MA . No evidence of association of heterozygous NTF4 mutations in patients with primary open-angle glaucoma. Am J Hum Genet 2010; 86 (3): 498–499.
Rao KN, Kaur I, Parikh RS, Mandal AK, Chandrasekhar G, Thomas R et al. Variations in NTF4, VAV2, and VAV3 genes are not involved with primary open-angle and primary angle-closure glaucomas in an indian population. Invest Ophthalmol Vis Sci 2010; 51: 4937–4941.
Cheng L, Sapieha P, Kittlerova P, Hauswirth WW, Di Polo A . TrkB gene transfer protects retinal ganglion cells from axotomy-induced death in vivo. J Neurosci 2002; 22: 3977–3986.
Cohen A, Bray GM, Aguayo AJ . Neurotrophin-4/5 (NT-4/5) increases adult rat retinal ganglion cell survival and neurite outgrowth in vitro. J Neurobiol 1994; 25: 953–959.
Rudzinski M, Wong TP, Saragovi HU . Changes in retinal expression of neurotrophins and neurotrophin receptors induced by ocular hypertension. J Neurobiol 2004; 58: 341–354.
Taylor S, Srinivasan B, Wordinger RJ, Roque RS . Glutamate stimulates neurotrophin expression in cultured Muller cells. Brain Res Mol Brain Res 2003; 111: 189–197.
Takahata K, Katsuki H, Kume T, Nakata D, Ito K, Muraoka S et al. Retinal neuronal death induced by intraocular administration of a nitric oxide donor and its rescue by neurotrophic factors in rats. Invest Ophthalmol Vis Sci 2003; 44: 1760–1766.
Rohrer B, LaVail MM, Jones KR, Reichardt LF . Neurotrophin receptor TrkB activation is not required for the postnatal survival of retinal ganglion cells in vivo. Exp Neurol 2001; 172 (1): 81–91.
Copin B, Brezin AP, Valtot F, Dascotte JC, Béchetoille A, Garchon HJ . Apolipoprotein E-promoter single-nucleotide polymorphisms affect the phenotype of primary open-angle glaucoma and demonstrate interaction with the myocilin gene. Am J Hum Genet 2002; 70: 1575–1581.
Lin HJ, Tsai FJ, Chen WC, Shi YR, Hsu Y, Tsai SW . Association of tumour necrosis factor alpha -308 gene polymorphism with primary open-angle glaucoma in Chinese. Eye 2003; 17: 31–34.
Shibuya E, Meguro A, Ota M, Kashiwagi K, Mabuchi F, Iijima H et al. Association of Toll-like receptor 4 gene polymorphisms with normal tension glaucoma. Invest Ophthalmol Vis Sci 2008; 49: 4453–4457.
Aung T, Ocaka L, Ebenezer ND, Morris AG, Krawczak M, Thiselton DL et al. A major marker for normal tension glaucoma: association with polymorphisms in the OPA1 gene. Hum Genet 2002; 110: 52–56.
Lin HJ, Chen WC, Tsai FJ, Tsai SW . Distributions of p53 codon 72 polymorphism in primary open angle glaucoma. Br J Ophthalmol 2002; 86: 767–770.
Vincent AL, Billingsley G, Buys Y, Levin AV, Priston M, Trope G et al. Digenic inheritance of early-onset glaucoma: CYP1B1, a potential modifier gene. Am J Hum Genet 2002; 70: 448–460.
Vasiliou V, Gonzalez FJ . Role of CYP1B1 in glaucoma. Annu Rev Pharmacol Toxicol 2008; 48: 333–358.
Fingert JH, Robin AL, Stone JL, Roos B, Davis LK, Scheetz TA et al. Copy number variations on chromosom 12q14 patients with Normal tension glaucoma. Hum Mol Genet 2011; 20: 2482–2494.
Meguro A, Inoko H, Ota M, Mizuki N, Bahram S . Genomewide association study of normal tension glaucoma: common variants in SRBD1 and ELOVL5 contribute to disease susceptibility. Ophthalmology 2010; 117: 1331–1338.e1335.
Rhee DJ, Haddadin RI, Kang MH, Oh DJ . Matricellular proteins in the trabecular meshwork. Exp Eye Res 2009; 88: 694–703.
Rhee DJ, Fariss RN, Brekken R, Sage EH, Russell P . The matricellular protein SPARC is expressed in human trabecular meshwork. Exp Eye Res 2003; 77: 601–607.
Chua J, Seet LF, Jiang Y, Su R, Htoon HM, Charlton A et al. Increased SPARC expression in primary angle closure glaucoma iris. Mol Vis 2008; 14: 1886–1892.
Seet LF, Su R, Barathi VA, Lee WS, Poh R, Heng YM et al. SPARC deficiency results in improved surgical survival in a novel mouse model of glaucoma filtration surgery. PLoS ONE 2010; 5: e9415.
Aroca-Aguilar J-D, Sanchez-Sanchez F, Ghosh S, Fernández-Navarro A, Coca-Prados M, Escribano J . Interaction of Recombinant Myocilin with the Matricellular Protein SPARC: Functional Implications. ARVO: Fort Lauderdale, Florida, 2010.
Chen LJ, Tam PO, Tham CC, Liang XY, Chiang SW, Canlas O et al. Evaluation of SPARC as a candidate gene of juvenile-onset primary open-angle glaucoma by mutation and copy number analyses. Mol Vis 2010; 16: 2016–2025.
Gonzalez P, Epstein DL, Borras T . Characterization of gene expression in human trabecular meshwork using single-pass sequencing of 1060 clones. Invest Ophthalmol Vis Sci 2000; 41: 3678–3693.
Berta AI, Kiss AL, Kemeny-Beke A, Lukats A, Szabó A, Szél A . Different caveolin isoforms in the retina of melanoma malignum affected human eye. Mol Vis 2007; 13: 881–886.
Ju H, Zou R, Venema VJ, Venema RC . Direct interaction of endothelial nitric-oxide synthase and caveolin-1 inhibits synthase activity. J Biol Chem 1997; 272: 18522–18525.
García-Cardeña G, Martasek P, Masters BS, Skidd PM, Couet J, Li S et al. Dissecting the interaction between nitric oxide synthase (NOS) and caveolin. Functional significance of the nos caveolin binding domain in vivo. J Biol Chem 1997; 272: 25437–25440.
Razani B, Zhang XL, Bitzer M, von Gersdorff G, Böttinger EP, Lisanti MP . Caveolin1 regulates transforming growth factor (TGF) beta/SMAD Signaling through an interaction with the TGF-beta type 1 receptor. J Biol Chem 2001; 276: 6727–6738.
Fuchshofer R, Tamm ER . Modulation of extracellular matrix turnover in the trabecular meshwork. Exp Eye Res 2009; 88: 683–688.
Toda N, Nakanishi-Toda M . Nitric oxide: ocular blood flow, glaucoma, and diabetic retinopathy. Prog Retin Eye Res 2007; 26: 205–238.
Kuehn MH, Wang K, Roos B, Stone EM, Kwon YH, Alward WL et al. Chromosome 7q31 POAG locus: ocular expression of caveolins and lack of association with POAG in a US cohort. Mol Vis 2011; 17: 430–435.
Burdon KP, Macgregor S, Hewitt AW, Sharma S, Chidlow G, Mills RA et al. Genome-wide association study identifies susceptibility loci for open angle glaucoma at TMCO1 and CDKN2B-AS1. Nat Genet 2011; 43: 574–578.
Porter LF, Urquhart JE, O’Donoghue E, Spencer AF, Wade EM, Manson FD et al. Identification of a novel locus for autosomal dominant primary open angle glaucoma on 4q35.1-q35.2. Invest Ophthalmol Vis Sci 2011; 52: 7859–7865.
Gottesman II, Shields J . Schizophrenia and Genetics: A Twin Study Vantage Point. Academic Press: New York, 1972.
Gottesman II, Shields J . Genetic theorizing and schizophrenia. Br J Psychiatry 1973; 122: 15–30.
Gershon ES, Goldin LR . Clinical methods in psychiatric genetics, I: robustness of genetic marker investigative strategies. Acta Psychiatr Scand 1986; 74: 113–118.
Leboyer M, Bellivier F, Nosten-Bertrand M, Jouvent R, Pauls D, Mallet J . Psychiatric genetics: search for phenotypes. Trends Neurosci 1998; 21: 102–105.
Desronvil T, Logan-Wyatt D, Abdrabou W, Triana M, Jones R, Taheri S . Distribution of COL8A2 and COL8A1 gene variants in Caucasian primary open angle glaucoma patients with thin central corneal thickness. Mol Vis 2010; 16: 2185–2191.
Leske MC, Heijl A, Hyman L, Bengtsson B, Dong L, Yang Z, EMGT Group. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology 2007; 114: 1965–1972.
Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 714–720, discussion 829–730.
Brandt JD, Beiser JA, Kass MA, Gordon MO . Central corneal thickness in the Ocular Hypertension Treatment Study (OHTS). Ophthalmology 2001; 108: 1779–1788.
Klein BE, Klein R, Lee KE . Heritability of risk factors for primary open-angle glaucoma: the Beaver Dam Eye Study. Invest Ophthalmol Vis Sci 2004; 45: 59–62.
Coote MA, McCartney PJ, Wilkinson RM, Mackey DA . The GIST score ranking glaucoma for genetic studies. Ophthalmic Genet 1996; 17: 199–208.
Duggal P, Klein AP, Lee KE, Iyengar SK, Klein R, Bailey-Wilson JE et al. Identification of Novel Genetic Loci for Intraocular Pressure: A Genome-wide Scan of the Beaver Dam Eye Study. Arch Ophthalmol 2007; 125: 74–79.
Vithana EN, Aung T, Khor CC, Cornes BK, Tay WT, Sim X et al. Collagen-related genes influence the glaucoma risk factor, central corneal thickness. Hum Mol Genet 2011; 20: 649–658.
Khor CC, Ramdas WD, Vithana EN, Cornes BK, Sim X, Tay WT et al. Genome-wide association studies in Asians confirm the involvement of ATOH7 and TGFBR3, and further identify CARD10 as a novel locus influencing optic disc area. Hum Mol Genet 2011; 20: 1864–1872.
Yang Z, Quigley HA, Pease ME, Yang Y, Qian J, Valenta D et al. Changes in gene expression in experimental glaucoma and optic nerve Transaction: the equilibrium between protective and detrimental mechanisms. Invest Ophthalmol Vis Sci 2007; 48: 5539–5548.
Hernandez MR . The optic nerve head in glaucoma: role of astrocytes in tissue remodeling. Prog Retin Eye Res 2000; 19: 297–321.
Murphy JA, Clarke DB . Target-derived neurotrophins may influence the survival of adult retinal ganglion cells when local neurotrophic support is disrupted: Implications for glaucoma. Med Hypotheses 2006; 67: 1208–1212.
Sawai H, Clarke DB, Kittlerova P, Bray GM, Aguayo AJ . Brain-derived neurotrophic factor and neurotrophin-4/5 stimulate growth of axonal branches from regenerating retinal ganglion cells. J Neurosci 1996; 16: 3887–3894.
Wax MB . The case for autoimmunity in glaucoma. Exp Eye Res 2011; 93: 187–190.
Li M, Xu J, Chen X, Sun X . RNA interference as a gene silencing therapy for mutant MYOC protein in primary open angle glaucoma. Diagn Pathol 2009; 4: 46.
Novina CD, Sharp PA . The RNAi revolution. Nature 2004; 430: 161–164.
Sontheimer EJ, Carthew RW . Molecular biology. Argonaute journeys into the heart of RISC. Science 2004; 305: 1409–1410.
Caplen NJ . Gene therapy progress and prospects. Downregulating gene expression: the impact of RNA interference. Gene Ther 2004; 11: 1241–1248.
Elbashir SM, Harborth J, Lendeckel W, Yalcin A, Weber K, Tuschl T . Duplexes of 21-nucleotide RNAs mediate RNA interference in cultured mammalian cells. Nature 2001; 411: 494–498.
Joe MK, Sohn S, Hur W, Moon Y, Choi YR, Kee C . Accumulation of Mutant myocilins in ER leads to ER stress and potential cytotoxicity in human trabecular meshwork cells. Biochem Biophys Res Commun 2003; 312: 592–600.
Yam GH, Gaplovska-Kysela K, Zuber C, Roth J . Aggregated myocilin induces russell bodies and causes apoptosis: implications for the pathogenesis of myocilin-caused primary open angle glaucoma. Am J Pathol 2007; 170: 100–109.
Ennis S, Gibson J, Griffiths H, Bunyan D, Cree AJ, Robinson D et al. Prevalence of myocilin gene mutations in a novel UK cohort of POAG patients. Eye 2010; 24: 328–333.
Mader N . Population at risk: glaucoma with focus on populations in the Americas. Ocular Surg News 2003; 22: 70–74.
Zhu X, Tang H, Risch N . Admixture mapping and the role of population structure for localizing disease genes. Adv Genet 2008; 60: 547–569.
Reich D, Patterson N . Will admixture mapping work to find disease genes? Phil Trans R Soc B 2005; 360: 1605–1607.
Cirruli ET, Goldstein DB . Uncovering the roles of rare variants in common disease through whole-genome sequencing. Nat Rev Genet 2010; 11: 415–425.
Bhattacharjee A, Acharya M, Mukhopadhyay A, Mookherjee S, Banerjee D, Bandopadhyay AK et al. Myocilin variants in Indian patients with open-angle glaucoma. Arch Ophthalmol 2007; 125: 823–829.
Mengkegale M, Fuse N, Miyazawa A, Takahashi K, Seimiya M, Yasui T et al. Presence of myocilin sequence variants in Japanese patients with open-angle glaucoma. Mol Vis 2008; 14: 413–417.
Fuse N, Takahashi K, Akiyama H, Nakazawa T, Seimiya M, Kuwahara S et al. Molecular genetic analysis of optineurin gene for primary open-angle and normal tension glaucoma in the Japanese population. J Glaucoma 2004; 13: 299–303.
Weisschuh N, Neumann D, Wolf C, Wissinger B, Gramer E . Prevalence of myocilin and optineurin sequence variants in German normal tension glaucoma patients. Mol Vis 2005; 11: 284–287.
Miyazawa A, Fuse N, Mengkegale M, Ryu M, Seimiya M, Wada Y et al. Association between primary open-angle glaucoma and WDR36 DNA sequence variants in Japanese. Mol Vis 2007; 13: 1912–1919.
Vickers JC, Craig JE, Stankovich J, McCormack GH, West AK, Dickinson JL et al. The apolipoprotein epsilon4 gene is associated with elevated risk of normal tension glaucoma. Mol Vis 2002; 8: 389–393.
Mabuchi F, Tang S, Ando D, Yamakita M, Wang J, Kashiwagi K et al. The apolipoprotein E gene polymorphism is associated with open angle glaucoma in the Japanese population. Mol Vis 2005; 11: 609–612.
Ressiniotis T, Griffiths PG, Birch M, Keers SM, Chinnery PF . Apolipoprotein E promoter polymorphisms do not have a major influence on the risk of developing primary open angle glaucoma. Mol Vis 2004; 10: 805–807.
Lake S, Liverani E, Desai M, Casson R, James B, Clark A et al. Normal tension glaucoma is not associated with the common apolipoprotein E gene polymorphisms. Br J Ophthalmol 2004; 88: 491–493.
Fan BJ, Liu K, Wang DY, Tham CC, Tam PO, Lam DS et al. Association of polymorphisms of tumor necrosis factor and tumor protein p53 with primary open-angle glaucoma. Invest Ophthalmol Vis Sci 2010; 51: 4110–4116.
Bozkurt B, Mesci L, Irkec M, Ozdag BB, Sanal O, Arslan U et al. Association of tumour necrosis factor alpha-308 G/A polymorphism with primary open-angle glaucoma. Clin Experiment Ophthalmol; e-pub ahead of print 17 May 2011; doi:10.1111/j.1442-9071.2011.02595.x.
Mabuchi F, Tang S, Kashiwagi K, Yamagata Z, Iijima H, Tsukahara S . The OPA1 gene polymorphism is associated with normal tension and high tension glaucoma. Am J Ophthalmol 2007; 143 (1): 125–130.
Woo SJ, Kim DM, Kim JY, Park SS, Ko HS, Yoo T . Investigation of the association between OPA1 polymorphisms and normal-tension glaucoma in Korea. J Glaucoma 2004; 13 (6): 492–495.
Daugherty CL, Curtis H, Realini T, Charlton JF, Zareparsi S . Primary open angle glaucoma in a Caucasian population is associated with the p53 codon 72 polymorphism. Molecular Vision 2009; 15: 1939–1944.
Fan BJ, Liu K, Wang DY, Tham CC, Tam PO, Lam DS et al. Association of polymorphisms of tumor necrosis factor and tumor protein p53 with primary open-angle glaucoma. Invest Ophthalmol Vis Sci 2010; 51: 4110–4116.
Mabuchi F, Sakurada Y, Kashiwagi K, Yamagata Z, Iijima H, Tsukahara S . Lack of association between p53 gene polymorphisms and primary open angle glaucoma in the Japanese population. Mol Vis 2009; 15: 1045–1049.
Silva RE, Arruda JT, Rodrigues FW, Moura KK . Primary open angle glaucoma was not found to be associated with p53 codon 72 polymorphism in a Brazilian cohort. Genet Mol Res 2009; 8: 268–272.
Melki R, Colomb E, Lefort N, Brézin AP, Garchon HJ . CYP1B1 mutations in French patients with early-onset primary open-angle glaucoma. J Med Genet 2004; 41: 647–651.
Chakrabarti S, Devi KR, Komatireddy S, Kaur K, Parikh RS, Mandal AK et al. Glaucoma-associated CYP1B1 mutations share similar haplotype backgrounds in POAG and PACG phenotypes. Invest Ophthalmol Vis Sci 2007; 48: 5439–5444.
Pasutto F, Chavarria-Soley G, Mardin CY, Michels-Rautenstrauss K, Ingelman-Sundberg M, Fernández-Martínez L et al. Heterozygous loss-of-function variants in CYP1B1 predispose to primary open-angle glaucoma. Invest Ophthalmol Vis Sci 2010; 51: 249–254.
Kuehn MH, Wang K, Roos B, Stone EM, Kwon YH, Alward WL et al. Chromosome 7q31 POAG locus: ocular expression of caveolins and lack of association with POAG in a US cohort. Mol Vis 2011; 17: 430–435.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gemenetzi, M., Yang, Y. & Lotery, A. Current concepts on primary open-angle glaucoma genetics: a contribution to disease pathophysiology and future treatment. Eye 26, 355–369 (2012). https://doi.org/10.1038/eye.2011.309
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.309
Keywords
This article is cited by
-
Effect of genotype on individual response to the pharmacological treatment of glaucoma: a systematic review and meta-analysis
Biology Direct (2023)
-
The C/A functional polymorphism of TGF-β2 gene (rs991967) in primary open angle glaucoma patients
Molecular Biology Reports (2023)
-
Visual field progression in Malay patients with primary glaucoma: survival analysis and prognostic factors
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)
-
Analysing the change in contrast sensitivity post-travoprost treatment in primary open-angle glaucoma patients using Spaeth Richman contrast sensitivity test
International Ophthalmology (2022)
-
Are we ready for genetic testing for primary open-angle glaucoma?
Eye (2018)