Abstract
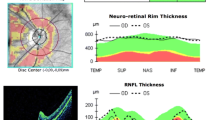
Purpose To investigate topographical relationship between amplitude of multifocal visual evoked potentials (mfVEP) and retinal nerve fibre layer (RNFL) thickness following acute optic neuritis (ON). Patients and Methods Fifty patients with a clinical diagnosis of acute unilateral ON between 6 and 36 months prior to the study and 25 age-matched controls underwent mfVEP testing (Accumap V 2.1, ObjectiVision Pty Ltd, Sydney, Australia) and OCT imaging (fast RNFL protocol, Stratus™, software version 3.0, Carl Zeiss Meditec, Inc., Dublin, CA). RNFL thickness and mfVEP amplitude were measured for upper, temporal and lower retinal sectors and corresponding areas of the visual field in affected eyes of ON patients and control eyes. Inter-eye asymmetry coefficients for both RNFL thickness and mfVEP amplitude were calculated for each zone, and corresponding coefficients were correlated between each other. Results There was highly significant reduction of RNFL thickness and mean mfVEP amplitude in all three retinal sectors of the affected eye. Largest reduction of RNFL thickness was noticed in temporal sector and of mfVEP amplitude in corresponding central part of the visual field. RNFL thickness correlated highly with amplitude of the mfVEP derived from corresponding areas of the visual field in all three zones. Conclusions We demonstrated strong topographical associations between structural and functional measures of optic nerve integrity in patients with ON.



Similar content being viewed by others
References
Tintore M, Rovira A, Rio J et al (2005) Is optic neuritis more benign than other first attacks in multiple sclerosis. Ann Neurol 57:210–215. doi:10.1002/ana.20363
Beck RW, Trobe JD, Moke PS et al (2003) High- and low-risk profiles for the development of multiple sclerosis within 10 years after optic neuritis: experience of the optic neuritis treatment trial. Arch Ophthalmol 121:944–949. doi:10.1001/archopht.121.7.944
Ghezzi A, Martinelli V, Torri V et al (1999) Long-term follow-up of isolated optic neuritis: the risk of developing multiple sclerosis, its outcome, and the prognostic role of paraclinical tests. J Neurol 246:770–775. doi:10.1007/s004150050453
Rodriguez M, Siva A, Cross SA et al (1995) Optic neuritis: a population-based study in Olmsted County, Minnesota. Neurology 45:244–250
Lassmann H (2005) Pathology of neurons in multiple sclerosis. In: SG Waxman (ed) Multiple sclerosis as a neuronal disease. Elsevier, Amsterdam, pp 153–164
Trapp BD, Peterson J, Ransohoff RM et al (1998) Axonal transection in the lesions of multiple sclerosis. N Engl J Med 338:278–285. doi:10.1056/NEJM199801293380502
Kornek B, Storch MK, Weissert R et al (2000) Multiple sclerosis and chronic autoimmune encephalomyelitis: a comparative study of axonal injury in active, inactive and remyelinated lesions. Am J Pathol 157:267–276
Youl BD, Turano G, Miller DH et al (1991) The pathophysiology of acute optic neuritis. An association of gadolinium leakage with clinical and electrophysiological deficits. Brain 114:2437–2450. doi:10.1093/brain/114.6.2437
Kallenbach K, Fredericksen JL (2007) Optical coherence tomography in optic neuritis and multiple sclerosis: a review. Eur J Neurol 14:841–849. doi:10.1111/j.1468-1331.2007.01736.x
Sergott RC, Frohman EM, Glanzman R, Al-Sabbagh A (2007) Optical coherence tomography in multiple sclerosis: expert panel consensus. J Neurol Sci 263:3–14
Trip A, Schlottmann PG, Jones SJ et al (2006) Optic nerve atrophy and retinal nerve fibre layer thinning following optic neuritis: Evidence that axonal loss is a substrate of MRI-detected atrophy. Neuroimage 31:286–293. doi:10.1016/j.neuroimage.2005.11.051
Quigley HA, Davis EB, Anderson DR (1977) Descending optic nerve degeneration in primates. Invest Ophthalmol Vis Sci 16:841–849
Trip A, Schlottmann PG, Jones SJ et al (2005) Retinal nerve fiber layer loss and visual disfunction in optic neuritis. Ann Neurol 58:383–391. doi:10.1002/ana.20575
Costello F, Coupland S, Zackon D et al (2005) Measurement of axon loss with optical coherence tomography in patients with optic neuritis. North American Neuro-Opthalmology society meeting proceedings, p 188
Parisi V, Manni G, Spadaro M et al (1999) Correlation between morphological and functional retinal impairment in multiple sclerosis patients. Invest Ophthalmol Vis Sci 40:2520–2527
Sergott RC (2005) Optical coherence tomography: measuring in vivo axonal survival and neuroprotection in multiple sclerosis and optic neuritis. Curr Opin Ophthalmol 16:346–350. doi:10.1097/01.icu.0000188705.67815.0e
Fisher JB, Jacobs DA, Markowitz CE et al (2006) Relation of visual function to retinal nerve fiber layer thickness in multiple sclerosis. Ophthalmology 113:324–332
Henderson A, Trip A, Schlottmann PG et al (2008) An investigation of the retinal nerve fibre layer in progressive multiple sclerosis using optical coherence tomography. Brain Pathol 131:277–287
Nuver MR (2006) Evoked potentials. In: Cook SD (ed) Handbook on multiple sclerosis. Taylor and Francis, New York, pp 243–269
Jones SJ, Brusa A (2003) Neurophysiological evidence for long-term repair of MS lesions: implications for axon protection. J Neurol Sci 206:193–198. doi:10.1016/S0022-510x(02)00428-8
Daniel P, Whittridge D (1961) The representation of the visual field on the cerebral cortex in monkeys. J Physiol 159:203–221
Riggs LA, Wooden BR (1972) Electrical measures and psychophysical data on human vision. In: Jamison D, Hurvich LM (eds) Handbook of sensory physiology, vol 7/4. Springer-Verlag, New York, pp 690–731
Yiannikas C, Walsh JC (1983) The variation of the pattern shift visual evoked response with the size of the stimulus field. Electroencephalogr Clin Neurophysiol 55:427–435. doi:10.1016/0013-4694(83)90131-1
Fraser C, Klistorner A, Graham SL et al (2006) Multifocal visual evoked potential latency analysis: predicting progression to multiple sclerosis. Arch Neurol 63:846–850
Baseler HA, Sutter EE, Klein SA, Carney T (1994) The topography of visual evoked response properties across the visual field. Electroencephalogr Clin Neurophysiol 90:65–81. doi:10.1016/0013-4694(94)90114-7
Klistorner AI, Graham SL, Grigg JR, Billson FA (1998) Multifocal topographic visual evoked potential: improving objective detection of local visual field defects. Invest Ophthalmol Vis Sci 39:937–950
Hood DC, Ohri N, Bo Yang E et al (2005) Determining abnormal latencies of multifocal visual evoked potentials: a monocular analysis. Doc Ophthalmol 109:189–199. doi:10.1007/s10633-004-5512-0
Fraser C, Klistorner A, Graham SL et al (2006) Multifocal visual evoked potential analysis of inflammatory or demyelinating optic neuritis. Ophthalmology 113:315–323
Hood DC (2000) Assessing retinal function with the multifocal technique. Prog Retin Eye Res 19:607–646. doi:10.1016/S1350-9462(00)00013-6
Graham SL, Klistorner A, Goldberg I (2005) Clinical application of objective perimetry using multifocal VEP in glaucoma practice. Arch Ophthalmol 123:729–739. doi:10.1001/archopht.123.6.729
Hood DC, Thienprasiddhi P, Greenstein VC et al (2004) Detecting early to mild glaucomatous damage: a comparison of the multifocal VEP and automated perimetry. Invest Ophthalmol Vis Sci 45:492–498. doi:10.1167/iovs.03-0602
Hood DC, Zhang X, Greenstein VC et al (2000) An interocular comparison of the multifocal VEP: a possible technique for detecting local damage to the optic nerve. Invest Ophthalmol Vis Sci 41:1580–1587
Klistorner A, Fraser C, Garrick R et al (2007) Correlation between full-field and multifocal VEPs in optic neuritis. Doc Ophthalmol 116:19–27. doi:10.1007/s10633-007-9072-y
Ruseckaite R, Maddess T, Danta G et al (2005) Sparse multifocal stimuli for the detection of multiple sclerosis. Ann Neurol 57:904–913. doi:10.1002/ana.20504
Klistorner A, Graham SL, Fraser C et al (2007) Electrophysiological evidence for heterogeneity of lesions in optic neuritis. Invest Ophthalmol Vis Sci 48:4549–4556. doi:10.1167/iovs.07-0381
Hood DC, Odel JG, Zhang X (2000) Tracking the recovery of local optic nerve function after optic neuritis: a multifocal VEP study. Invest Ophthalmol Vis Sci 41:4032–4038
Noval S, Contreras I, Rebolleda G, Munoz-Negrete FJ (2006) Optical coherence tomography versus automated perimetry for follow-up of optic neuritis. Acta Ophthalmol Scand 84:790–794. doi:10.1111/j.1600-0420.2006.00724.x
Frohman EM, Costello F, Stuve O et al (2008) Modeling axonal degeneration within the anterior visual system. Ann Neurol 65:26–35
McDonald WI, Compston A, Edan G et al (2001) Recommended diagnostic criteria for multiple sclerosis: guidelines from the international panel on the diagnosis of the multiple sclerosis. Ann Neurol 50:121–127. doi:10.1002/ana.1032
Graham SL, Klistorner AI, Grigg JR, Billson FA (2000) Objective VEP perimetry in glaucoma: asymmetry analysis to identify early deficits. J Glaucoma 9:10–19
Klistorner A, Graham SL (2001) Electroencephalogram-based scaling of multifocal visual evoked potentials: effect on intersubject amplitude variability. Invest Ophthalmol Vis Sci 42:2145–2152
Goldberg I, Graham SL, Klistorner A (2002) Multifocal objective perimetry in the detection of glaucomatous field loss. Am J Ophthalmol 133:29–39. doi:10.1016/S0002-9394(01)01294-6
Klistorner AI, Graham SL, Grigg JR, Billson FA (1998) Electrode position and the multi-focal visual-evoked potential: role in objective visual field assessment. Aust NZ J Ophthalmol 26:91–94. doi:10.1111/j.1442-9071.1998.tb01386.x
Graham SL, Klistorner A (1999) The diagnostic significance of the multifocal pattern visual evoked potential in glaucoma. Curr Opin Ophthalmol 10:140–146. doi:10.1097/00055735-199904000-00011
Garway-Heath DF, Poinoosawmy D, Fitzke F, Hitchings RA (2000) Mapping the visual field to the optic disc in normal tension glaucoma eyes. Ophthalmology 107:1809–1815. doi:10.1016/S0161-6420(00)00284-0
Balachandran C, Graham SL, Klistorner A, Goldberg I (2006) Comparison of objective diagnostic tests in glaucoma: Heidelberg retinal tomography and multifocal visual evoked potentials. J Glaucoma 15:110–116. doi:10.1097/00061198-200604000-00006
Sepulcre J, Murie-Fernandez M, Salinas-Alaman A et al (2007) Diagnostic accuracy of retinal abnormalities in predicting disease activity in MS. Neurology 66:1488–1494. doi:10.1212/01.wnl.0000260612.51849.ed
Alamouti B, Funk J (2003) Retinal thickness decreases with age: an OCT study. Br J Ophthalmol 87:899–901. doi:10.1136/bjo.87.7.899
Paunescu LA, Schuman JS, Price LL et al (2004) Variation of nerve fibre layer thickness measurements with age and ethnicity by scanning laser polarimetry. Invest Ophthalmol Vis Sci 40:2520–2527
Hickman SJ, Toosy AT, Jones SJ et al (2004) A serial MRI study following optic nerve mean area in acute optic neuritis. Brain Pathol 127:2498–2505
Toosy AT, Hickman SJ, Mizszkiel KA et al (2005) Adaptive cortical plasticity in higher visual areas after optic neuritis. Ann Neurol 57:622–633. doi:10.1002/ana.20448
Smith KJ, Waxman SG (2005) The conduction properties of demyelinated and remyelinated axons. In: Waxman SG (ed) Multiple sclerosis as neuronal disease. Elsevier Academic Press, Amsterdam, pp 85–100
Kutzelnigg A, Lucchinetti CF, Stadelmann C et al (2005) Cortical demyelination and diffuse white matter injury in multiple sclerosis. Brain Pathol 128:2705–2712
Filippi M, Rocca M (2005) MRI evidence for multiple sclerosis as a diffuse disease of the central nervous system. J Neurol 252(Suppl):v16–v24. doi:10.1007/s00415-005-5004-5
Lassmann H (2007) New concepts on progressive multiple sclerosis. Cur Neurol Neurosci Rep 7:239–244
Parisi V, Manni G, Centofanti M et al (2001) Correlation between optical coherence tomography, pattern electroretinogram, and visual evoked potentials in open-angle glaucoma patients. Ophthalmology 108:905–912. doi:10.1016/S0161-6420(00)00644-8
Costello F, Coupland S, Hodge W et al (2006) Quantifying axonal loss after optic neuritis with optical coherent tomography. Ann Neurol 59:963–969. doi:10.1002/ana.20851
Kerrison JB, Flynn T, Green WR (1994) Retinal pathologic changes in multiple sclerosis. Retina 14:445–451. doi:10.1097/00006982-199414050-00010
Evangelou N, Konz D, Esiri MM et al (2001) Size-selective neuronal changes in the anterior optic pathways suggest a differential susceptibility to injury in multiple sclerosis. Brain 124:1813–1820. doi:10.1093/brain/124.9.1813
Budenz DL, Chang RT, Huang X et al (2005) Reproducibility of retinal nerve fiber thickness measurements using the stratus OCT in normal and glaucomatous eyes. Invest Ophthalmol Vis Sci 46:2440–2443. doi:10.1167/iovs.04-1174
Klistorner A, Graham SL (2006) Interest variability of mfVEP amplitude: reducing its effect on the interpretation of sequential tests. Doc Ophthalmol 111:159–167. doi:10.1007/s10633-005-5363-3
Klistorner A, Graham SL (2000) Objective perimetry in glaucoma. Ophthalmology 107:2283–2299
Acknowledgement
The study was supported by Sydney Medical Foundation and ORIA grants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Klistorner, A., Arvind, H., Nguyen, T. et al. Multifocal VEP and OCT in optic neuritis: a topographical study of the structure–function relationship. Doc Ophthalmol 118, 129–137 (2009). https://doi.org/10.1007/s10633-008-9147-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10633-008-9147-4