Abstract
Objective. Resection or even biopsy of an intra-axial mass lesion in close relationship to eloquent cortex carries a major risk of neurological deficit. We have assessed the safety and effectiveness of craniotomy under local anesthesia and monitored conscious sedation for the resection of tumors involving eloquent cortex.
Methods. We have performed a retrospective review of a consecutive series of 157 adult patients who underwent craniotomy under local anesthesia by one surgeon (P.M.B.) at Brigham and Women's Hospital in Boston. All patients had tumors in close proximity to eloquent cortex, including speech, motor, primary sensory, or visual cortex. In most cases the lesion was considered inoperable by the referring surgeon. All resection was verified by post-operative imaging approximately one month after surgery and all cases were reviewed by an independent neurosurgeon (A.D.).
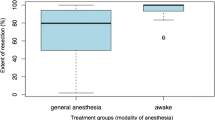
Results. In 122 cases, brain mapping was performed to identify eloquent cortex and in the remainder neurological monitoring was maintained during the procedure. Radiological gross total resection was achieved in 57% of patients and greater than 80% resection was achieved in 23%. Thus 4 out of 5 of patients had major resection despite the close relationship of tumor to eloquent cortex. In 13%, resection could be done but less than 80% of tumor was removed because of danger of neurological deficit. In 7% of patients, only a biopsy could be done because of infiltration into eloquent cortex that could only be assessed at surgery.
In 76 patients with pre-operative neurological deficits, there was complete resolution of these deficits in 33%, improvement in 32%, no change in 28%, and long-term worsening in 8%. Among 81 patients with no pre-operative neurological deficit, 1 patient suffered a major permanent neurological deficit, and 2 developed minor deficits. There was a transient post-operative deficit in one-third of cases, but this had resolved at one month in all but three patients.
Monitored conscious sedation was performed without anesthetic complications using midazolam, sufentanyl and fentanyl with or without propofol. Only one case needed to be converted to general anesthesia. Patient satisfaction with the procedure has been good. Operating time and hospital stay were lower than the mean for brain tumor craniotomy at this hospital.
Conclusions. Tumor surgery with conscious sedation is a safe technique that allows maximal resection of lesions in close anatomical relationship to eloquent cortex, with a low risk of new neurological deficit. Only 7% of intrinsic cortical tumors were ineligible for partial or complete resection with this technique.
Similar content being viewed by others
References
Berger MS, Cohen WA, Ojemann GA: Correlation of motor cortex brain mapping data with magnetic resonance imaging. J Neurosurg 72: 383-387, 1990
Haglund MM, Berger MS, Shamseldin M, Lettich E, Ojemann GA: Cortical localization of temporal lobe language sites in patients with gliomas. Neurosurgery 34: 567-576, 1994
Ojemann G, Ojemann J, Lettich B, Berger M: Cortical language localization in left, dominant hemisphere-an electrical stimulation mapping investigation in 117 patients. J Neurosurg 71: 316-326, 1989
Berger MS, Deliganis AV, Dobbins J, Keles GE: The effect of extent of resection on recurrence in patients with low grade cerebral hemisphere gliomas. Cancer 74: 1784-1791, 1994
Salcman M: The value of cytoreductive surgery. Clin Neurosurg 41: 464-488, 1994
Nikas D, Black PMcL: Neurosurgical management of low grade gliomas. Neurosur Focus, April 1998
Penfield W, Roberts L: Speech and Brain Mechanisms. Princeton University Press, Princeton, 1959
Van Buren JM, Fedio P, Frederick GC: Mechanism and localization of speech in the parietotemporal cortex. Neurosurgery 2: 223-239, 1978
Walsh AR, Ojemann GA: Anterior temporal lobectomy for epilepsy. Clin Neurosurg 38: 535-547, 1991
Berger MS: Lesions in functional ('eloquent') cortex and subcortical white matter. Clin Neurosurg 41: 444-463, 1994
Berger MS, Kincaid J, Ojemann GA, Lettich E: Brain mapping techniques to maximize resection, safety, and seizure control in children with brain tumors. Neurosurgery 25: 786-792, 1989
Black PM, Ronner SF: Cortical mapping for defining the limits of tumor resection. Neurosurgery 20: 914-919, 1987
Ebeling U, Schmid UD, Ying H, Reulen HJ: Safe surgery of lesions near the motor cortex using intra-operative mapping techniques: a report on 50 patients. Acta Neurochirugica (Wien) 119: 23-28, 1992
Gregorie EM, Goldring S: Localization of function in the excision of lesions from the sensorimotor region. J Neurosurg 61: 1047-1054, 1984
Walsh AR, Schmidt RH, Marsh HT: Cortical mapping and local anesthetic resection as an aid to surgery of low and intermediate gliomas. Br J Neurosurg 6: 119-124, 1992
Gleason PL, Kikinis R, Altobelli D, Wells W, Alexander E, Black PM, Jolesz F: Video registration virtual reality for nonlinkage stereotactic surgery. Stereotact Funct Neurosurg 63: 139-143, 1994
Kikinis R, Gleason PL, Moriarty TM, Moore MR, Steig PE, Matsumae M, Lorensen WE, Cline HE, Black PM, Jolesz FA: Computer assisted, interactive, three-dimensional neurosurgical planning. Neurosurgery 1995
Chabrerie A, Ozlen F, Nakajima S, Leventon ME, Atsumi H, Grimson E, Jolesz F, Kikinis R, Black PM: Three-dimensional image reconstruction for low-grade glioma surgery. Neurosurg Focus 4(4): Article 7, 1998
Taylor MD, Bernstein M: A wake craniotomy with brain mapping as the routine surgical approach to treating patients with supratentorial intraaxial tumors: a prospective trial of 200 cases. J Neurosurg 90(1): 35-41, 1999
Silbergeld DL, Mueller WM, Colley PS, Ojemann GA, Lettich E: Use of propofol (diprivan) for awake craniotomies: technical note. Surg Neurol 38: 271-272, 1992
Manninen P, Contreras J: Anesthetic considerations for craniotomy in the awake patient. Int Anesthesiology Clinics (United States) 24: 157-174, 1986
Welling EC, Donegan J: Neuroleptanalgesia using alfentanil for awake craniotomy. Anesth Analg 68: 57-60, 1989
Adelson PD, Black PM, Madsen JR, Kramer U, Rockoff MA, Riviello JJ, Helmers SL, Mikati M, Holmes GL: The use of subdural grids and strip electrodes to identify a seizure focus in children. Pediatric Neurosurg 22: 174-180, 1995
Gugino LS, Aglio L, Black P: Intraoperative monitoring. In Kaye A, Black P (eds) Operative Neurosurgery, London, Churchill Livingstone, 1999
Puce A, Constable T, Luby ML, McCarthy G, Nobre AC, Spencer DD, Gore JC, Allison T: Functional magnetic resonance imaging of sensory and motor cortex: comparison with electrophysiological localization. J Neurosurg 83: 262-270, 1995
Fried I, Nenov VI, Ojemann SG, Woods RP: Functional MRI and PET imaging of rolandic and visual cortices for neurosurgical planning. J Neurosurg 83: 854-861, 1995
Gallen CC, Schwartz BJ, Bucholz RD, Malik G, Barkley GL, Smith J, Tung H, Copeland B, Bruno L, Assam S: Presurgical localization of functional cortex using magnetic source imaging. J Neurosurg 82: 988-994, 1995
Gallen CC, Sobel DF, Waltz T, Aung M, Copeland B, Schwartz BJ, Hirschkoff EC, Bloom FE: Noninvasive presurgical neuromagnetic mapping of somatosensory cortex. Neurosurgery 33: 260-268, 1993
Yousry TA, Schmid UD, Jassoy AG, Schmidt D, Bisner WD, Reulen HJ, Reiser MF, Lissner J: Topography of the cortical motor hand area: a prospective study with functional MR imaging and motor mapping at surgery. Radiology 195: 23-29, 1995
Nimsky C, Ganslandt O, Kober H, Moller M, Ulmer S, Tomandi B, Fahlbusch R: Integration of functional magnetic resonance imaging supported by magnetoencephalography in functional neuronavigation. Neurosurgery 44(6): 1249-1255, 1999
Danks RA, Rogers M, Aglio LS, Gugino LD, Black PM: Patient tolerance of craniotomy performed with the patient under local anesthesia and monitored conscious sedation. Neurosurgery 42(1): 28-36 1998
Nikas DC, Bello L, Zamani AA, Black PM: Neurosurgical considerations in supratentorial low-grade gliomas: experience with 175 patients. Neurosurg Focus 4(4): Article 4, 1998
Chabrerie A, Ozlen F, Nakajima S, Leventon M, Atsumi H, Grimson E, Jolesz F, Kikinis R, Black PM: Three-dimensional image reconstruction for low-grade glioma surgery. Neurosurg Focus 4(4): Article 7, 1998.
Martin C, Alexander III E, Wong T, Schwartz R, Jolesz F, Black P: Surgical treatment of low-grade gliomas in the intraoperative magnetic resonance imager. Neurosurg Focus 4(4): Article 8, 1998.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Danks, R.A., Aglio, L.S., Gugino, L.D. et al. Craniotomy Under Local Anesthesia and Monitored Conscious Sedation for the Resection of Tumors Involving Eloquent Cortex. J Neurooncol 49, 131–139 (2000). https://doi.org/10.1023/A:1026577518902
Issue Date:
DOI: https://doi.org/10.1023/A:1026577518902