Abstract
Individuals over 80 years of age represent the most rapidly growing segment of the population, and late-life dementia has become a major public health concern worldwide. Development of effective preventive and treatment strategies for late-life dementia relies on a deep understanding of all the processes involved. In the centuries since the Greek philosopher Pythagoras described the inevitable loss of higher cognitive functions with advanced age, various theories regarding the potential culprits have dominated the field, ranging from demonic possession, through 'hardening of blood vessels', to Alzheimer disease (AD). Recent studies suggest that atrophy in the cortex and hippocampus—now considered to be the best determinant of cognitive decline with aging—results from a combination of AD pathology, inflammation, Lewy bodies, and vascular lesions. A specific constellation of genetic and environmental factors (including apolipoprotein E genotype, obesity, diabetes, hypertension, head trauma, systemic illnesses, and obstructive sleep apnea) contributes to late-life brain atrophy and dementia in each individual. Only a small percentage of people beyond the age of 80 years have 'pure AD' or 'pure vascular dementia'. These concepts, formulated as the dynamic polygon hypothesis, have major implications for clinical trials, as any given drug might not be ideal for all elderly people with dementia.
Key Points
-
Over the past 27 centuries, the perception of cognitive impairment with aging has changed from a normal inevitable part of aging to being mostly attributable to Alzheimer disease (AD)
-
Alois Alzheimer was one of the first clinician–scientists to describe the importance of vascular pathology and to de-emphasize the role of amyloid plaques in brain atrophy and late-life dementia
-
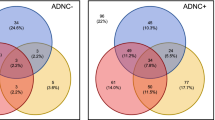
Clinicopathological studies have consistently shown that individuals over 80 years of age generally have 'mixed' pathologies (infarcts, plaques, tangles, Lewy bodies and inflammation) rather than 'pure AD'
-
The size of the cortex and hippocampus—more than AD or any other single pathological finding—correlates with the degrees of cognitive decline and dementia in elderly individuals
-
Appreciating the link between midlife risk factors and late-life size of the cortex and hippocampus has serious implications for disease diagnosis, patient management, and interpretation of research findings
-
The dynamic polygon hypothesis provides a new framework for thinking about aging and dementia that departs from the linear model proposed by the amyloid cascade hypothesis
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Berchtold, N. C. & Cotman, C. W. Evolution in the conceptualization of dementia and Alzheimer's disease: Greco-Roman period to the 1960s. Neurobiol. Aging 19, 173–189 (1998).
Mast, H., Tatemichi, T. K. & Mohr, J. P. Chronic brain ischemia: the contributions of Otto Binswanger and Alois Alzheimer to the mechanisms of vascular dementia. J. Neurol. Sci. 132, 4–10 (1995).
Alzheimer, A. On peculiar cases of disease at higher age [German]. Neurologie und Psychiatrie 4, 256–286 (1911).
Ballenger, J. F. Progress in the history of Alzheimer's disease: the importance of context. J. Alzheimers Dis. 9, 5–13 (2006).
Wilson, D. C. The pathology of senility. Am. J. Psychiatry 111, 902–906 (1955).
Hachinski, V. C., Lassen, N. A. & Marshall, J. Multi-infarct dementia. A cause of mental deterioration in the elderly. Lancet 2, 207–210 (1974).
Blessed, G., Tomlinson, B. E. & Roth, M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. Br. J. Psychiatry 114, 797–811 (1968).
Hardy, J. A. & Higgins, G. A. Alzheimer's disease: the amyloid cascade hypothesis. Science 256, 184–185 (1992).
Cummings, J. L. Alzheimer's disease. N. Engl. J. Med. 351, 56–67 (2004).
Hardy, J. & Selkoe, D. J. The amyloid hypothesis of Alzheimer's disease: progress and problems on the road to therapeutics. Science 297, 353–356 (2002).
McKhann, G. et al. Clinical diagnosis of Alzheimer's disease: report of the NINCDS–ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology 34, 939–944 (1984).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th edn (American Psychiatric Association, Washington, D. C., 1994).
Khachaturian, Z. S. Diagnosis of Alzheimer's disease. Arch. Neurol. 42, 1097–1105 (1985).
Mirra, S. S. et al. The Consortium to Establish a Registry for Alzheimer's Disease (CERAD). Part II. Standardization of the neuropathologic assessment of Alzheimer's disease. Neurology 41, 479–486 (1991).
Jellinger, K. A. Criteria for the neuropathological diagnosis of dementing disorders: routes out of the swamp? Acta Neuropathol. 117, 101–110 (2009).
Braak, H. & Braak, E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 82, 239–259 (1991).
[No authors listed] Consensus recommendations for the postmortem diagnosis of Alzheimer's disease. The National Institute on Aging, and Reagan Institute Working Group on Diagnostic Criteria for the Neuropathological Assessment of Alzheimer's Disease. Neurobiol. Aging 18 (4 Suppl.), S1–S2 (1997).
McKeith, I. G. Dementia with Lewy bodies. Br. J. Psychiatry 180, 144–147 (2002).
McKeith, I. G. et al. Consensus guidelines for the clinical and pathologic diagnosis of dementia with Lewy bodies (DLB): report of the Consortium on DLB International Workshop. Neurology 47, 1113–1124 (1996).
Hachinski, V. et al. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke 37, 2220–2241 (2006).
Relkin, N., Marmarou, A., Klinge, P., Bergsneider, M. & Black, P. M. Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery 57 (3 Suppl.), S4–S16 (2005).
Yoshimura, M. et al. Dementia in cerebral amyloid angiopathy: a clinicopathological study. J. Neurol. 239, 441–450 (1992).
Nagy, Z. et al. The effects of additional pathology on the cognitive deficit in Alzheimer disease. J. Neuropathol. Exp. Neurol. 56, 165–170 (1997).
Erkinjuntti, T., Ostbye, T., Steenhuis, R. & Hachinski, V. The effect of different diagnostic criteria on the prevalence of dementia. N. Engl. J. Med. 337, 1667–1674 (1997).
Petersen, R. C. et al. Mild cognitive impairment: clinical characterization and outcome. Arch. Neurol. 56, 303–308 (1999).
Petersen, R. C. & Negash, S. Mild cognitive impairment: an overview. CNS Spectr. 13, 45–53 (2008).
Snowdon, D. A. et al. Brain infarction and the clinical expression of Alzheimer disease. The Nun Study. JAMA 277, 813–817 (1997).
Viswanathan, A., Rocca, W. A. & Tzourio, C. Vascular risk factors and dementia: how to move forward? Neurology 72, 368–374 (2009).
Neuropathology Group. Medical Research Council Cognitive Function and Aging Study. Pathological correlates of late-onset dementia in a multicentre, community-based population in England and Wales. Neuropathology Group of the Medical Research Council Cognitive Function and Ageing Study (MRC CFAS). Lancet 357, 169–175 (2001).
Fotuhi, M. Preserving memory: tips to help baby boomers stay in the game. Practical Neurology March/April, 34–40 (2009).
Troncoso, J. C. et al. Effect of infarcts on dementia in the Baltimore longitudinal study of aging. Ann. Neurol. 64, 168–176 (2008).
Kivipelto, M. et al. Obesity and vascular risk factors at midlife and the risk of dementia and Alzheimer disease. Arch. Neurol. 62, 1556–1560 (2005).
Kivipelto, M. et al. Risk score for the prediction of dementia risk in 20 years among middle aged people: a longitudinal, population-based study. Lancet Neurol. 5, 735–741 (2006).
Aguero-Torres, H., Kivipelto, M. & von Strauss, E. Rethinking the dementia diagnoses in a population-based study: what is Alzheimer's disease and what is vascular dementia? A study from the Kungsholmen project. Dement. Geriatr. Cogn. Disord. 22, 244–249 (2006).
Prohovnik, I. et al. Dissociation of neuropathology from severity of dementia in late-onset Alzheimer disease. Neurology 66, 49–55 (2006).
White, L. et al. Recent clinical–pathologic research on the causes of dementia in late life: update from the Honolulu–Asia Aging Study. J. Geriatr. Psychiatry Neurol. 18, 224–227 (2005).
Schmitt, F. A. et al. “Preclinical” AD revisited: neuropathology of cognitively normal older adults. Neurology 55, 370–376 (2000).
Crystal, H. A. et al. The relative frequency of “dementia of unknown etiology” increases with age and is nearly 50% in nonagenarians. Arch. Neurol. 57, 713–719 (2000).
Nelson, P. T., Braak, H. & Markesbery, W. R. Neuropathology and cognitive impairment in Alzheimer disease: a complex but coherent relationship. J. Neuropathol. Exp. Neurol. 68, 1–14 (2009).
Korczyn, A. D. The amyloid cascade hypothesis. Alzheimers Dement. 4, 176–178 (2008).
Schneider, J. A., Arvanitakis, Z., Bang, W. & Bennett, D. A. Mixed brain pathologies account for most dementia cases in community-dwelling older persons. Neurology 69, 2197–2204 (2007).
Savva, G. M. et al. Age, neuropathology, and dementia. N. Engl. J. Med. 360, 2302–2309 (2009).
White, L. Brain lesions at autopsy in older Japanese-American men as related to cognitive impairment and dementia in final years of life: a summary report from the Honolulu–Asia Aging Study. J. Alzheimers Dis. doi:10.3233/JAD-2009-1178.
Schneider, J. A., Arvanitakis, Z., Leurgans, S. E. & Bennett, D. A. The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann. Neurol. 66, 200–208 (2009).
Sonnen, J. A. et al. Pathological correlates of dementia in a longitudinal, population-based sample of aging. Ann. Neurol. 62, 406–413 (2007).
Haroutunian, V. et al. Role of the neuropathology of Alzheimer disease in dementia in the oldest-old. Arch. Neurol. 65, 1211–1217 (2008).
Erten-Lyons, D. et al. Factors associated with resistance to dementia despite high Alzheimer disease pathology. Neurology 72, 354–360 (2009).
Jagust, W. J. et al. Neuropathological basis of magnetic resonance images in aging and dementia. Ann. Neurol. 63, 72–80 (2008).
Helzner, E. P. et al. Contribution of vascular risk factors to the progression in Alzheimer disease. Arch. Neurol. 66, 343–348 (2009).
Korf, E. S., White, L. R., Scheltens, P. & Launer, L. J. Midlife blood pressure and the risk of hippocampal atrophy: the Honolulu Asia Aging Study. Hypertension 44, 29–34 (2004).
Du, A. T. et al. Age effects on atrophy rates of entorhinal cortex and hippocampus. Neurobiol. Aging 27, 733–740 (2006).
Sapolsky, R. M. Chickens, eggs and hippocampal atrophy. Nat. Neurosci. 5, 1111–1113 (2002).
Sapolsky, R. M. Depression, antidepressants, and the shrinking hippocampus. Proc. Natl Acad. Sci. USA 98, 12320–12322 (2001).
Knecht, S. et al. Atrial fibrillation in stroke-free patients is associated with memory impairment and hippocampal atrophy. Eur. Heart J. 29, 2125–2132 (2008).
den Heijer, T. et al. Type 2 diabetes and atrophy of medial temporal lobe structures on brain MRI. Diabetologia 46, 1604–1610 (2003).
Appenzeller, S., Carnevalle, A. D., Li, L. M., Costallat, L. T. & Cendes, F. Hippocampal atrophy in systemic lupus erythematosus. Ann. Rheum. Dis. 65, 1585–1589 (2006).
Tate, D. F. & Bigler, E. D. Fornix and hippocampal atrophy in traumatic brain injury. Learn. Mem. 7, 442–446 (2000).
Biessels, G. J., De Leeuw, F. E., Lindeboom, J., Barkhof, F. & Scheltens, P. Increased cortical atrophy in patients with Alzheimer's disease and type 2 diabetes mellitus. J. Neurol. Neurosurg. Psychiatry 77, 304–307 (2006).
Sheline, Y. I., Gado, M. H. & Kraemer, H. C. Untreated depression and hippocampal volume loss. Am. J. Psychiatry 160, 1516–1518 (2003).
Barnes, D. E. et al. Predicting risk of dementia in older adults. The late-life dementia risk index. Neurology 73, 173–179 (2009).
Jefferson, A. L. et al. Lower cardiac output is associated with greater white matter hyperintensities in older adults with cardiovascular disease. J. Am. Geriatr. Soc. 55, 1044–1048 (2007).
Kril, J. J., Patel, S., Harding, A. J. & Halliday, G. M. Patients with vascular dementia due to microvascular pathology have significant hippocampal neuronal loss. J. Neurol. Neurosurg. Psychiatry 72, 747–751 (2002).
Gustafson, D. Adiposity indices and dementia. Lancet Neurol. 5, 713–720 (2006).
Wiseman, R. M. et al. Hippocampal atrophy, whole brain volume, and white matter lesions in older hypertensive subjects. Neurology 63, 1892–1897 (2004).
Minoguchi, K. et al. Silent brain infarction and platelet activation in obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 175, 612–617 (2007).
Macey, P. M. et al. Brain morphology associated with obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 166, 1382–1387 (2002).
Whitmer, R. A. et al. Central obesity and increased risk of dementia more than three decades later. Neurology 71, 1057–1064 (2008).
Diano, S. et al. Ghrelin controls hippocampal spine synapse density and memory performance. Nat. Neurosci. 9, 381–388 (2006).
LeRoith, D. Insulin-like growth factors and the brain. Endocrinology 149, 5951 (2008).
Neumann, K. F. et al. Insulin resistance and Alzheimer's disease: molecular links & clinical implications. Curr. Alzheimer Res. 5, 438–447 (2008).
Yaffe, K. et al. The metabolic syndrome, inflammation, and risk of cognitive decline. JAMA 292, 2237–2242 (2004).
Farrer, L. A. et al. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. APOE and Alzheimer Disease Meta Analysis Consortium. JAMA 278, 1349–1356 (1997).
Tiraboschi, P. et al. Impact of APOE genotype on neuropathologic and neurochemical markers of Alzheimer disease. Neurology 62, 1977–1983 (2004).
Drzezga, A. et al. Effect of APOE genotype on amyloid plaque load and gray matter volume in Alzheimer disease. Neurology 72, 1487–1494 (2009).
Cheng, D. et al. Functional interaction between APOE4 and LDL receptor isoforms in Alzheimer's disease. J. Med. Genet. 42, 129–131 (2005).
Berlau, D. J., Corrada, M. M., Head, E. & Kawas, C. H. APOE ε2 is associated with intact cognition but increased Alzheimer pathology in the oldest old. Neurology 72, 829–834 (2009).
Cotman, C. W., Berchtold, N. C. & Christie, L. A. Exercise builds brain health: key roles of growth factor cascades and inflammation. Trends Neurosci. 30, 464–472 (2007).
Helzner, E. P., Scarmeas, N., Cosentino, S., Portet, F. & Stern, Y. Leisure activity and cognitive decline in incident Alzheimer disease. Arch. Neurol. 64, 1749–1754 (2007).
Neeper, S. A., Gomez-Pinilla, F., Choi, J. & Cotman, C. W. Physical activity increases mRNA for brain-derived neurotrophic factor and nerve growth factor in rat brain. Brain Res. 726, 49–56 (1996).
Adlard, P. A., Perreau, V. M., Pop, V. & Cotman, C. W. Voluntary exercise decreases amyloid load in a transgenic model of Alzheimer's disease. J. Neurosci. 25, 4217–4221 (2005).
Erickson, K. I. et al. Training-induced plasticity in older adults: effects of training on hemispheric asymmetry. Neurobiol. Aging 28, 272–283 (2007).
Colcombe, S. J. et al. Aerobic exercise training increases brain volume in aging humans. J. Gerontol. A Biol. Sci. Med. Sci. 61, 1166–1170 (2006).
Draganski, B. et al. Temporal and spatial dynamics of brain structure changes during extensive learning. J. Neurosci. 26, 6314–6317 (2006).
Drachman, D. A. Aging of the brain, entropy, and Alzheimer disease. Neurology 67, 1340–1352 (2006).
Drachman, D. A. Nature or nurture: education and the trajectory of declining brain function with age and Alzheimer disease. Neurology 70, 1725–1727 (2008).
McGurn, B., Deary, I. J. & Starr, J. M. Childhood cognitive ability and risk of late-onset Alzheimer and vascular dementia. Neurology 71, 1051–1056 (2008).
Ambrée, O. et al. Reduction of amyloid angiopathy and Aβ plaque burden after enriched housing in TgCRND8 mice: involvement of multiple pathways. Am. J. Pathol. 169, 544–552 (2006).
Hartman, R. E. et al. Pomegranate juice decreases amyloid load and improves behavior in a mouse model of Alzheimer's disease. Neurobiol. Dis. 24, 506–515 (2006).
Fotuhi, M., Mohassel, P. & Yaffe, K. Fish consumption, long-chain omega-3 fatty acids and risk of cognitive decline or Alzheimer disease: a complex association. Nat. Clin. Pract. Neurol. 5, 140–152 (2009).
Yang, L. et al. Inhibition of the expression of prostate specific antigen by curcumin [Chinese]. Yao Xue Xue Bao 40, 800–803 (2005).
Chan, A. & Shea, T. B. Dietary supplementation with apple juice decreases endogenous amyloid-β levels in murine brain. J. Alzheimers Dis. 16, 167–171 (2009).
Kivipelto, M. & Solomon, A. Preventive neurology: on the way from knowledge to action. Neurology 73, 168–169 (2009).
Aizenstein, H. J. et al. Frequent amyloid deposition without significant cognitive impairment among the elderly. Arch. Neurol. 65, 1509–1517 (2008).
Mathis, C. A. Amyloid imaging fundings from multicenter studies. Alzheimers Dement. 5, IC-S1-01 (2009).
van der Flier, W. M. & Scheltens, P. Alzheimer disease: hippocampal volume loss and Alzheimer disease progression. Nat. Rev. Neurol. 5, 361–362 (2009).
Driscoll, I. et al. Longitudinal pattern of regional brain volume change differentiates normal aging from MCI. Neurology 72, 1906–1913 (2009).
Salmond, C. H. et al. Diffusion tensor imaging in chronic head injury survivors: correlations with learning and memory indices. Neuroimage 29, 117–124 (2006).
Cummings, J. L., Doody, R. & Clark, C. Disease-modifying therapies for Alzheimer disease: challenges to early intervention. Neurology 69, 1622–1634 (2007).
Salloway, S. & Correia, S. Alzheimer disease: time to improve its diagnosis and treatment. Cleve. Clin. J. Med. 76, 49–58 (2009).
Fillit, H., Hess, G., Hill, J., Bonnet, P. & Toso, C. IV immunoglobulin is associated with a reduced risk of Alzheimer disease and related disorders. Neurology 73, 180–185 (2009).
Holmes, C. et al. Long-term effects of Aβ42 immunisation in Alzheimer's disease: follow-up of a randomised, placebo-controlled phase I trial. Lancet 372, 216–223 (2008).
Hardy, J. The amyloid hypothesis for Alzheimer's disease: a critical reappraisal. J. Neurochem. 110, 1129–1134 (2009).
Jack, C. R. Jr, et al. Serial PIB and MRI in normal, mild cognitive impairment and Alzheimer's disease: implications for sequence of pathological events in Alzheimer's disease. Brain 132, 1355–1365 (2009).
Giannakopoulos, P. et al. Tangle and neuron numbers, but not amyloid load, predict cognitive status in Alzheimer's disease. Neurology 60, 1495–1500 (2003).
Jagust, W. Will neuroimaging help us understand Alzheimer's disease? Alzheimer's & Dementia 5, IC-PL-01 (2009).
Shankar, G. M. et al. Amyloid-β protein dimers isolated directly from Alzheimer's brains impair synaptic plasticity and memory. Nat. Med. 14, 837–842 (2008).
Lee, H. G. et al. Amyloid-β in Alzheimer disease: the null versus the alternate hypotheses. J. Pharmacol. Exp. Ther. 321, 823–829 (2007).
Seabrook, G. R., Ray, W. J., Shearman, M. & Hutton, M. Beyond amyloid: the next generation of Alzheimer's disease therapeutics. Mol. Interv. 7, 261–270 (2007).
Abbott, A. Neuroscience: the plaque plan. Nature 456, 161–164 (2008).
Small, S. A. & Duff, K. Linking Aβ and tau in late-onset Alzheimer's disease: a dual pathway hypothesis. Neuron 60, 534–542 (2008).
Williams, M. Progress in Alzheimer's disease drug discovery: an update. Curr. Opin. Investig. Drugs 10, 23–34 (2009).
Fotuhi, M. et al. Better cognitive performance in elderly taking antioxidant vitamins E and C supplements in combination with nonsteroidal anti-inflammatory drugs: the Cache County Study. Alzheimers Dement. 4, 223–227 (2008).
Trachtenberg, D. I. & Trojanowski, J. Q. Dementia: a word to be forgotten. Arch. Neurol. 65, 593–595 (2008).
Hachinski, V. World Stroke Day 2008: “little strokes, big trouble”. Stroke 39, 2407–2420 (2008).
Hachinski, V. Shifts in thinking about dementia. JAMA 300, 2172–2173 (2008).
Knopman, D. S. Go to the head of the class to avoid vascular dementia and skip diabetes and obesity. Neurology 71, 1046–1047 (2008).
Kivipelto, M. & Solomon, A. Cholesterol as a risk factor for Alzheimer's disease—epidemiological evidence. Acta Neurol. Scand. Suppl. 185, 50–57 (2006).
Kivipelto, M., Solomon, A., Blennow, K., Olsson, A. G. & Winblad, B. The new cholesterol controversy—a little bit of history repeating? Acta Neurol. Scand. Suppl. 185, 1–2 (2006).
Acknowledgements
V. Hachinski is funded by the Alzheimer Association, Award Number IIRG-08-91792. P. J. Whitehouse received support from the National Institute on Aging, Shigeo and Megumi Takayama, and the Greenwall Foundation. Barbara Crain, Miia Kivipelto and Michael Williams made significant suggestions, and we very much appreciate their critical and thoughtful comments. We thank Tzipora Sofare, Medical Editor at the Sandra and Malcolm Berman Brain & Spine Institute, for her help with the preparation of the tables and figures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Table 1
Studies reflecting the heterogeneity of neuropathological findings in elderly people over the age of 80 years, with or without dementia. (DOC 66 kb)
Rights and permissions
About this article
Cite this article
Fotuhi, M., Hachinski, V. & Whitehouse, P. Changing perspectives regarding late-life dementia. Nat Rev Neurol 5, 649–658 (2009). https://doi.org/10.1038/nrneurol.2009.175
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2009.175
This article is cited by
-
Direct and indirect neurological, cognitive, and behavioral effects of COVID-19 on the healthy elderly, mild-cognitive-impairment, and Alzheimer’s disease populations
Neurological Sciences (2021)
-
Computational modeling of the effects of autophagy on amyloid-β peptide levels
Theoretical Biology and Medical Modelling (2020)
-
Risk of dementia in patients with end-stage renal disease under maintenance dialysis—a nationwide population-based study with consideration of competing risk of mortality
Alzheimer's Research & Therapy (2019)
-
Effects of a new nutraceutical combination on cognitive function in hypertensive patients
Immunity & Ageing (2018)
-
Clinical dementia severity associated with ventricular size is differentially moderated by cognitive reserve in men and women
Alzheimer's Research & Therapy (2018)