Summary
Abstract
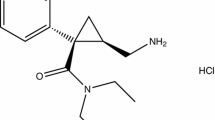
Milnacipran is a cyclopropane derivative which acts by inhibiting noradrenaline (norepinephrine) and serotonin (5-hydroxytryptamine; 5-HT) reuptake at presynaptic sites; no postsynaptic receptor activity has been demonstrated. It is most commonly administered at a dosage of 50mg twice daily for the treatment of major depressive disorder. Improvement usually occurs within 2 weeks of treatment initiation, but some patients do respond sooner.
Most studies which evaluated milnacipran were of short (4 to 8 weeks) duration and results were not published in full with rigorous peer review.
Nonetheless, the drug is significantly more effective than placebo for the treatment of in-or outpatients with moderate to severe major depressive disorder. Limited data suggest that it may prevent relapse and be effective for long term use, although this requires confirmation.
Milnacipran 200 mg/day is generally not significantly different from amitriptyline 150 mg/day in terms of onset and efficacy. However, when doses are titrated (not a requirement for milnacipran), milnacipran 50 or 100 mg/day has a slower onset than the tricyclic antidepressant. At a dosage of 100 mg/day for 4 to 12 weeks, milnacipran generally has similar efficacy to imipramine and clomipramine 150 mg/day, although milnacipran 50 to 150 mg/day had a faster onset of activity than imipramine 50 to 150 mg/day in Japanese patients. In a 6-month trial, milnacipran was less effective than clomipramine.
Milnacipran 50 or 100mg twice daily was as effective as fluoxetine 20mg once daily or fluvoxamine 100mg twice daily in 4-to 12-week studies. At a dosage of 50 then 100mg daily it was also as effective as mianserin 30 then 60mg daily in a 4-week study. However, when administered once daily (in the evening), milnacipran 100 mg/day was not as effective as fluoxetine 20 mg/day after 6 weeks.
The drug is generally well tolerated, producing no more adverse events (including anticholinergic events) than placebo, selective serotonin reuptake inhibitors or mianserin and fewer adverse events than tricyclic antidepressants in clinical trials. However, dysuria has been reported in 7% of male patients receiving milnacipran.
Conclusions: Data from predominantly short term trials suggest that milnacipran generally has similar efficacy to tricyclic antidepressants and SSRIs. Although further published data are required to confirm its efficacy, good tolerability profile and pharmacokinetic profile which suggests a low potential for drug interactions, milnacipran should be considered a promising agent for the treatment of patients with major depressive disorder.
Pharmacodynamic Properties
Milnacipran is a cyclopropane derivative which appears to act at presynaptic sites to inhibit noradrenaline (norepinephrine) and serotonin (5-hydroxytryptamine; 5-HT) uptake. The inhibitory capacity of milnacipran is of approximately the same order as that of imipramine for noradrenaline and serotonin uptake in vitro and in vivo.
Milnacipran does not appear to act at any postsynaptic receptor in vitro or in vivo. In rats, it has no effect on β-adrenergic receptor density, function or affinity, postsynaptic 5-HT2 receptor numbers or sensitivity, adenylcyclase activity, α1-or α2-adrenergic, 5-HT1 or benzodiazepine receptors or monoamine A or B activity.
Behavioural tests based on interactions with the noradrenergic or serotonergic system showed milnacipran to be very active. The effective oral doses of milnacipran producing inhibition in 50% of mice involved in these tests were generally lower than those of tricyclic antidepressants.
Milnacipran 3 to 60 mg/kg produces dose-dependent antidepressant activity in the forced swimming test, in the conditioned fear stress test, after exposure to the uncontrollable aversion situation and during forced walking stress in rats and/or mice and reduces hyperactivity of olfactory bulbectomised rats in the ‘open field’ test. These effects, however, are usually significant only at doses of ≥30 mg/kg. Reductions in immobility time during the forced swimming test were associated with increases in interstitial serotonin levels in rats.
Compared with placebo, milnacipran 100 mg/day for 7 days had nonsignificant effects on cognitive function but appeared to improve deferred visual memory in healthy volunteers. The same dose of milnacipran for 3 days also had no significant effect when volunteers were given a small amount of alcohol (blood concentration of 0.5 g/L) before performing simulated driving testing. Tests examining short term memory, choice reaction time and quality of awakening in elderly volunteers showed milnacipran 75 mg/day for 3 days to have effects that were not significantly different from those of placebo. However, milnacipran had less effect on choice reaction time than amitriptyline 50 mg/day and improved critical flicker fusion test performance significantly when compared with both amitriptyline and placebo.
Milnacipran had negligible anticholinergic activity in behavioural models and this was reflected in studies of the cardiovascular effects of the drug. Intravenous milnacipran 0.2 to 0.8 mg/kg induced some cardiovascular changes in 10 healthy volunteers, but most were not considered important and occurred at plasma concentrations higher than those seen after a 100mg dose of the drug. Heart rate and systolic blood pressure increased, and the functional refractory periods of the atrium and atrioventricular node and the effective refractory period of the right ventricle decreased.
The cardiovascular effects of milnacipran were usually less severe or less numerous than those induced by tricyclic antidepressants (predominantly imipramine) in animals. In general, trends in electrocardiographic changes induced by milnacipran were small and difficult to qualify, although heart rate tended to increase.
Pharmacokinetic Properties
The pharmacokinetics of single oral doses of milnacipran have been investigated in 2 groups of 12 healthy volunteers. Milnacipran 50mg has a bioavailability of 85%. Maximum serum concentrations (Cmax) are dose-proportional for single doses of milnacipran 25 to 200mg, with the Cmax of a 50mg dose being 134 μg/L after 2 hours (tmax). After a 50mg dose, volume of distribution is 5.3 L/kg, area under the concentration-time curve (AUC) is 1833 μg/L · h, elimination half-life (t1/2) is 6.1 or 8.1 hours and total clearance is 37.6 L/h/1.73m2. Interindividual variation is low (except for tmax) and good correlation is demonstrated between single-dose and steady-state pharmacokinetics.
Oral milnacipran 50 or 100mg twice daily for 28 days had linear pharmacokinetics in 17 patients with major depressive disorder. At 2 hours, Cmax values of D- and L-milnacipran were 223 to 419 nmol/L after a 50mg dose and 381 to 690 nmol/L after a 100mg dose. Values of t1/2 (5 to 9 hours) appeared to be independent of dose and time. Steady-state concentrations of milnacipran are rapidly achieved (after 2 to 3 days with twice daily dosing) in healthy volunteers. Serotonin uptake inhibition parallels blood drug concentrations.
Milnacipran has low and nonsaturable binding to plasma proteins. This, and the fact that the drug is not metabolised by the hepatic cytochrome P450 (CYP) system, reduces the number of likely drug interactions involving milnacipran. First-pass metabolism is low and no active metabolites have been identified in humans. 50 to 60% of the drug is excreted unchanged. Milnacipran does not accumulate after multiple dosages.
The pharmacokinetics of milnacipran are not significantly affected by hepatic impairment. However, in patients with renal impairment [glomerular filtration rate of 9 to 85 ml/min (0.54 to 5.1 L/h)], changes in total and renal clearance are correlated with decreases in glomerular function. In these patients and in the elderly, Cmax values are increased and elimination is prolonged compared with in healthy volunteers and younger adults, respectively.
Therapeutic Use
To date, many of the trials assessing the efficacy of milnacipran in the treatment of depression, in particular those comparing the drug with other antidepressants, have been published only as abstracts or in summary papers.
In 3 double-blind multicentre placebo-controlled trials, milnacipran 50mg twice daily was significantly more effective than placebo for the treatment of in-or outpatients with major depressive disorder. Efficacy was measured using the Montgomery-Åsberg Depression Rating Scale (MADRS), Hamilton Depression Rating Scale (HDRS) and Clinical Global Impression (CGI) rating. The largest and longest placebo-controlled trial showed significantly more milnacipran than placebo recipients to respond to treatment (>50% decrease in HDRS total score from baseline) after 8 weeks (65 vs 44%. Dosages of 25 and 100mg twice daily were not as effective as the 50mg twice daily dosage.
Although some improvement has been observed with milnacipran as early as after 1 week, it usually occurs within 2 weeks of treatment initiation. Efficacy was maintained in 23 patients who received milnacipran 50 to 200 mg/day for 4 to 65 weeks. Limited evidence from 165 patients who received treatment for a mean of 21 weeks (all were treated for >8 weeks) also suggests that milnacipran may prevent relapse.
Milnacipran 50 or 100 mg/day had a slower onset of action than amitriptyline 150 mg/day in multicentre double-blind trials which enrolled patients with major depressive disorder, but the efficacy of milnacipran 100 mg/day and amitriptyline were similar after 4 weeks. Dosages of both drugs were titrated to the levels specified over 5 days, although this is not necessary for milnacipran. A higher dosage of milnacipran (200 mg/day) was not significantly different from amitriptyline at any time according to total MADRS, HDRS, CGI severity of illness or efficacy index scores. However, improvements in CGI global improvement scores were significantly larger in milnacipran recipients than in amitriptyline-treated patients at 7 and 28 days.
There were no significant differences in changes in HDRS and/or MADRS scores for milnacipran 100 mg/day and imipramine or clomipramine 150 mg/day recipients according to the results of individual 4-to 12-week studies and pooled data from 7 trials (842 patients with major depressive disorder). One trial included elderly (65 to 90 years) patients only, and there were also no significant between-treatment differences in efficacy in this population. However, results of a longer (26-week) trial indicated that although some advantages for milnacipran 200 mg/day were seen in terms of good tolerability, the drug was significantly less effective than clomipramine 150 mg/day in adult in-or outpatients with depression.
Patients with melancholia appear to be particularly responsive to milnacipran. A trial, as yet published only as part of a review, showed no significant differences at 12 weeks between milnacipran 50mg twice daily (n = 93) and fluoxetine 20mg once daily (n = 100) according to HDRS and MADRS scores and the proportion of responders, although milnacipran had a faster onset of action. Unpublished results indicate that an additional 96 patients received milnacipran 100mg twice daily in this study; the efficacy of this regimen was not significantly different from that of the other two. However, milnacipran 100 mg/day, when administered as a single evening dose to patients with major depressive disorder, was not as effective as fluoxetine 20 mg/day after 6 weeks. The dosage regimen of milnacipran used in this study of 190 patients was unusual and probably sub-optimal (milnacipran has a short half-life and no active metabolites). No significant differences were noted between recipients of milnacipran 150mg twice daily for 2 weeks followed by 75mg twice daily (n = 41), milnacipran 100mg twice daily (n = 42) or fluvoxamine 100mg twice daily (n = 37) in 4-week MADRS, HDRS or CGI scores or the number of patients who responded to therapy.
After 4 weeks, the efficacy of milnacipran 50 then 100mg daily was not significantly different from that of mianserin 30 then 60mg daily in Japanese patients, but efficacy was noted sooner in milnacipran recipients.
Tolerability
Milnacipran, most commonly at a dosage of 100 or 200 mg/day, was generally well tolerated and usually produced no more adverse events (including anticho-linergic events) than placebo in clinical trials.
In comparative trials, anticholinergic effects (dry mouth, blurred vision) occurred significantly more frequently with amitriptyline, clomipramine or imipramine than with milnacipran. However, insomnia during the first 6 weeks of treatment, dyspnoea and treatment for constipation were significantly more common with milnacipran than clomipramine in 26-week trials. Milnacipran had a better overall tolerability profile than tricyclic antidepressants, but its tolerability profile was not significantly different from that of fluoxetine, fluvoxamine or mianserin in a small number of trials. Analysis of several comparative trials showed that milnacipran was associated with significantly fewer cardiovascular events and withdrawals because of poor tolerability than tricyclic antidepressants. Events most frequently causing withdrawal of milnacipran were gastrointestinal disturbances, dysuria and palpitations. Indeed, dysuria, which occurred at ahigher frequency with milnacipran than with tricyclic antidepressants, has been reported to occur in 7% of male patients receiving milnacipran.
A database of clinical trials involving milnacipran (n = 1871) showed that vertigo, increased sweating, anxiety, hot flushes and dysuria occurred in significantly more milnacipran than placebo recipients (n = 394). However, dry mouth, constipation, tremor, sweating, somnolence, tiredness and vertigo all occurred at a significantly greater incidence with tricyclic antidepressants (n = 940) than with milnacipran. The incidence of nausea was significantly higher with the SSRIs fluoxetine and fluvoxamine (n = 344) than with milnacipran. However, dysuria was significantly more common with milnacipran than with tricyclic antidepres-sants or SSRIs.
In general, the most commonly reported adverse events in Japanese patients were anticholinergic (dry mouth, constipation and, less frequently, urinary retention, nasal obstruction or dryness and visual disturbances), gastrointestinal, or dizziness or headache. Less frequently, orthostatic hypotension, drowsiness and rash occurred.
Laboratory abnormalities were infrequently reported and were not serious. Unpublished data show that milnacipran had no electrocardiographic effects in 939 patients.
Dosage and Administration
The optimal dosage of milnacipran is 50mg twice daily for the treatment of patients with major depressive disorder in European countries. However, in Japan, the optimal dosage is 25mg twice daily; 15mg twice daily is recommended for elderly patients in this country.
Dosage reduction is necessary in patients with impaired renal function, but not in those with hepatic impairment.
Similar content being viewed by others
References
Viazzo P, Alphand V, Furstoss R. Microbiological transformations 34: enantioselective hydrolysis of a key-lactone involved in the synthesis of the antidepressant milnacipran®. Tetrahedron Lett 1996; 37(26): 4519–22
Moret C, Charveron M, Finberg JP, et al. Biochemical profile of midalcipran (F 2207), 1-phenyl-1-diethyl-aminocarbonyl-2-aminomethyl-cyclopropane (Z) hydrochloride, a potential fourth generation antidepressant drug. Neuropharmacology 1985 Dec; 24: 1211–9
Assie M-B, Broadhurst A, Briley M. Is down-regulation of β-adrenoceptors necessary for antidepressant activity? In: Briley M, Fillion G, editors. New concepts in depression. London: Mac Millan Press, 1988: 161–6
Assie MB, Charveron M, Palmier C, et al. Effects of prolonged administration of milnacipran, a new antidepressant, on receptors and monoamine uptake in the brain of the rat. Neuropharmacology 1992 Feb; 31: 149–55
Matsubara R, Matsubara S, Koyama T, et al. Effect of chronic treatment with milnacipran (TN-912), a novel antidepressant, on beta-adrenergic receptor-adenylate cyclase system and serotonin 2 receptor in the rat cerebral cortex [in Japanese]. Jpn J Neuropsychopharmacol 1993; 15(2): 119–26
Moret C, Briley M. Effect of antidepressant drugs on monoamine synthesis in brain in. vivo. Neuropharmacology 1992 Jul; 31: 679–84
Kitamura Y, Nagatani T, Takao K, et al. Pharmacological study of milnacipran, a novel antidepressant [in Japanese]. Jpn J Neuropsychopharmacol 1995; 17(1): 25–34
Palmier C, Puozzo C, Lenehan T, et al. Monoamine uptake inhibition by plasma from healthy volunteers after single oral doses of the antidepressant milnacipran. EurJ Clin Pharmacol 1989 Sep; 37: 235–8
Moret C, Briley M. Milnacipran, a double noradrenaline and 5-HT reuptake inhibiting antidepressant increases cerebral extracellular monoamine levels [abstract no. P.1.024]. Eur Neuropsychopharmacol 1996 Sep; 6 Suppl. 4: S4–68
de Montigny C, Mongeau R, Weiss M, et al. The antidepressant drug milnacipran modulates 5-HT neuron activity via the noradrenergic system [abstract no. 103.10]. 24th Annual Meeting of the Society of Neuroscience; 1994 Nov 13–18; Florida, USA, 226
Barone P, Moret C, Briley M, et al. Autoradiographic characterization of binding sites for [3H]milnacipran, a new antidepressant drug, and their relationship to the serotonin transporter in rat brain. Brain Res 1994 Dec 30; 668: 129–43
Moret C. Serotonergic autoreceptor and antidepressants [in French]. Psychiatr Psychobiol 1990; 5(3): 195–9
Neliat G, Bodinier M-C, Panconi E, et al. Lack of effect of repeated administration of milnacipran, a double noradrenaline and serotonin reuptake inhibitor, on the β-adrenoceptor-linked adenylate cyclase system in the rat cerebral cortex. Neuropharmacology 1996; 35(5): 589–93
Moret C, Briley M. Effect of milnacipran and desipramine on noradrenergic α2-autoreceptor sensitivity. Prog Neuropsychopharmacol Biol Psychiatry 1994 Oct; 18: 1063–72
Stenger A, Couzinier J-P, Briley M. Psychopharmacology of midalcipran, l-phenyl-1-diethyl-amino-carbonyl-2-aminomethyl-cyclopropane hydrochloride (F 2207), a new potential antidepressant. Psychopharmacology Berl 1987; 91: 147–53
Laval J, Stenger A, Briley M. Involvement of both α1- and β-adrenoceptors in the antagonism of tetrabenazine-induced effects by antidepressants. In: Briley M, Fillion G, editors. New concepts in depression. London: MacMillan Press, 1988: 211–5
Bonnaud B, Cousse H, Mouzin G, et al. l-Aryl-2-(aminomethyl)cyclopropanecarboxylic acid derivatives. A new series of potential antidepressants. J Med Chem 1987 Feb; 30: 318–25
Stenger A, Laval J, Couret E, et al. Behavioral changes in mice after acute and chronic imipramine or milnacipran treatment [abstract]. Eur J Pharmacol 1990 Jul 5; 183: 1907
Serre C, Elphick M, Grahame-Smith D, et al. Lack of anticho-linergic action of midalcipran compared to amitriptyline in normal subjects [abstract no. 32.05.28]. Psychopharmacology 1988; 96 Suppl: 273
Hashimoto S, Inoue T, Koyama T. Serotonin reuptake inhibitors reduced conditioned fear stress-induced freezing behavior in rats. Psychopharmacology 1996; 123: 182–6
Sasaki N, Nara K, Murata S, et al. In. vivoneurochemical effects of milnacipran on forced swimming of the rat [abstract]. Psychiatr Clin Neurosci 1996 Apr; 50: S82
Redmond AM, Kelly JP, Leonard BE. The behavioural effects of milnacipran in the olfactory bulbectomised rat model of depression. Med Sci Res 1995 Aug; 23: 533–4
Lacroix P, Rocher N, Gandon JM, et al. Antidepressant effects of milnacipran in the learned helplessness test in rats [abstract]. Eur Neuropsychopharmacol 1995 Sep; 5 Spec. Issue: 276
Kitayama I, Nomura J. Effect of maprotiline and milnacipran on the spontaneous activity and brain catecholamine of the stress-induced depression-model rats [abstract]. Jpn J Psychiatry Neurol 1994 Sep; 48: 700–1
Poirier MF, Galinowski A, Longevialle R, et al. Etude comparative du milnacipran (2) versus placebo sur les fonctions congitives chez des volontaires sains [abstract]. 3éme Conférence Vigilance et Performances Psychomotrices; 1991 Apr 8–9; Annecy, France.
Hindmarch I, Orluc A, Serre C. Etude des effets du milnacipran (F 2207) sur les fonctions sensori–et psycho-motrices du volontaires sain age de plus de 60 ans [abstract]. Association Francaise de Psychiatrie Biologique; 1989 May 20
Hindmarch I, Alford C, Barwell F, et al. Measuring the side effects of psychotropics: the behavioural toxicity of antide-pressants. J Psychopharmacol 1992; 6(2): 198–203
Richet F, Marais J, Serre C, et al. Etude comparative en double aveugle milnacipran et placebo avec et sans alcool sur la vigilance et la conduite automobile de volontaires sains [abstract]. 3éme Conférence Vigilance et Performances Psychomotrices; 1991 Apr 8–9; Annecy, France.
Caron J, Libersa C, Hazard JR, et al. Acute electrophysiological effects of intravenous milnacipran, a new antidepressant agent. Eur Neuropsychopharmacol 1993 Dec; 3: 493–500
Kawasaki H, Yamamoto R, Urabe M, et al. Electroencephalo-graphic and cardiovascular effects of milnaciplan hydrochlo-ride (TN-912), a novel antidepressant [in Japanese]. Folia Pharmacol Jpn 1991 Nov; 98: 345–55
Rouet RH, Tisne-Versailles J, Adamantidis MM, et al. Comparative invivoand invitrostudy of the cardiac effects of midalcipran and imipramine. Fundam Clin Pharmacol 1989; 3: 237–44
Puozzo C, Rostin M, Montastruc JL, et al. Absolute bioavailability study of midalcipran (F 2207) in volunteers [abstract]. Third European Congress of Biopharmaceutics and Pharmacokinetics Proceedings; 1987 Apr 21–24; Freiburg, Switzerland.
Puozzo C, Filaquier C, Briley M. Plasma levels of F 2207, midalcipran, a novel antidepressant, after single oral administration in volunteers [abstract]. Br J Clin Pharmacol 1985; 20: 291P
Retz W, Becker T, Schmidtke A, et al. Multiple and single dose pharmacokinetics of milnacipran in major depressive patients [abstract]. Eur Neuropsychopharmacol 1995 Sep; 5 Spec. Issue: 296–7
Puozzo C, Lambe R, Filaquier C, et al. Plasma levels and (3H)-5HT uptake in platelets after human repeated administration of midalcipran [abstract]. Acta Pharmacol Toxicol 1986; 59: 214
Puozzo C, Leonard BE. Pharmacokinetics of milnacipran in comparison with other antidepressants. Int Clin Psychopharmacol 1996 Sep; 11 Suppl. 4: 15–27
Takahashi A, Kawaguchi T, Kasahara T, et al. Absorption and excretion study of milnacipran hydrochloride in healthy volunteers, a 15mg tablet. Influence of food intake and multiple oral administration [in Japanese]. Rinsho Iyaku 1995; 11 (5) Suppl. 3: 119–32
Puozzo C, Lambe R, Briley M. Pharmacokinetic-pharmacodynamic relationship of milnacipran on platelet uptake model [abstract]. Eur Neuropsychopharmacol 1996 Apr; 6 Suppl. 1: S17
Puozzo C, Albin H, Vinçon G, et al. Pharmacokinetics of milnacipran in liver impairment [abstract]. Eur J Drug Metab Pharmacokinet 1996; 21(2) Suppl.: 77
Benard P, Puozzo C, Roux C, et al. Transplacental passage and milk excretion of radioactivity in laboratory animals dosed with 14C-F 2207: a quantitative whole-body autoradiographic study. In: Baillie TA, Jones JR, editors. Synthesis and applications of isotopically labelled compounds. Proceedings of the Third International Symposium; 1988 Jul 17–21; Innsbruck, Austria. Amsterdam: Elsevier Science Publishers BV, 1988: 637–40
Puozzo C, Pozet N, Deprez D, et al. Pharmacokinetics of milnacipran in renal impairment [abstract]. Eur J Drug Metab Pharmacokinet 1996; 21(2) Suppl.: 78
Puozzo C, Deville G, Bromet-Petit M, et al. Single dose pharmacokinetics of F 2207, a new antidepressant drug, in elderly volunteers [abstract]. Symposium on variability in pharmacokinetics and drug response; 1988 Oct 3–5; Gothenburg, Sweden.
Ansseau M, von Frenckell R, Serre C. Pilot study of milnacipran in panic disorder. Eur Psychiatry 1991; 6(2): 103–5
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed., Washington, DC: American Psychiatric Association, 1980.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 3rd ed revised. Washington DC: American Psychiatric Association, 1987.
Hamilton M. Development of a rating scale for primary depressive illness. Brit J Soc Clin Psychol 1967; 6: 278–96
Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry 1979; 134: 382–9
Lecrubier Y, Pletan Y, Solles A, et al. Clinical efficacy of milnacipran: placebo-controlled trials. Int Clin Psychopharmacol 1996 Sep; 11 Suppl. 4: 29–33
Serre C, Clerc G, Escande M, et al. An early clinical trial of midalcipran, 1-phenyl-1-diethyl aminocarbonyl 2-aminomethyl cyclopropane (Z) hydrochloride, a potential fourth generation antidepressant. Curr Ther Res Clin Exp 1986; 39(1): 156–64
Ansseau M, von Frenckell R, Mertens C, et al. Controlled comparison of two doses of milnacipran (F 2207) and amitriptyline in major depressive inpatients. Psychopharmacology Berl 1989; 98: 163–8
Kawakatsu S, Totsuka S, Yoshimura E, et al. Clinical effectiveness of milnacipran hydrochloride by long-term administration study [in Japanese]. Rinsho Iyaku 1994; 10(12): 2715–36
Macher J-P, Sichel J-P, Serre C, et al. Double-blind placebocontrolled study of milnacipran in hospitalized patients with major depressive disorders. Neuropsychobiology 1989; 22(2): 77–82
Puech A, Montgomery SA, Prost JF, et al. Milnacipran, a new serotonin and noradrenaline reuptake inhibitor: an overview of its antidepressant activity and clinical tolerability. Int Clin Psychopharmacol 1997; 12: 99–108
Yamashita I, Matsubara R, Onodera I, et al. Clinical evaluation of milnacipran hydrochloride (TN-912) on depression and depressive states. Phase III clinical trial with imipramine hydrochloride as a control drug [in Japanese]. Rinsho Iyaku 1995; 11(4): 819–42
Ansseau M, Papart P, Troisfontaines B, et al. Controlled comparison of milnacipran and fluoxetine in major depression. Psychopharmacology 1994 Feb; 114: 131–7
Clerc G, Pagot R, Bouchard JM, et al. Therapeutic contribution of milnacipran and clomipramine during a 3-month treatment: results of a comparative study [in French]. Psychiatr Psychobiol 1990; 5(2): 137–43
Kasper S, Pletan Y, Solles A, et al. Comparative studies with milnacipran and tricyclic antidepressants in the treatment of patients with major depression: a summary of clinical trial results. Int Clin Psychopharmacol 1996 Sep; 11 Suppl. 4: 35–9
Steen A, Den Boer JA. A double-blind six months comparative study of milnacipran and clomipramine in major depressive disorder. Int Clin Psychopharmacol 1997; 12: 269–81
Leinonen E, Lepola U, Koponen H, et al. Long-term efficacy and safety of milnacipran compared to clomipramine in patients with major depression. Acta Psychiatr Scand 1997 Dec; 96: 497–504
Ansseau M, von Frenckell R, Gerard M-A, et al. Interest of a loading dose of milnacipran in endogenous depressive inpatients. Comparison with the standard regimen and with fluvoxamine. Eut Neuropsychopharmacol 1991 May; 1: 113–21
Ansseau M, von Frenckell R, Papart P, et al. Controlled comparison of milnacipran (F2207) 200 mg and amitriptyline in endogenous depressive inpatients. Hum Psychopharmacol 1989; 4(3): 221–7
Matsubara R, Onodera I, Ito K, et al. A double-blind comparison of milnacipran and imipramine in depressive patients [abstract]. Eur Neuropsychopharmacol 1996 Jun; 6 Suppl. 3: 48
Ferreri M. A double-blind comparison of the antidepressant actions of milnacipran and imipramine in major depressive disorder. Institut de Recherche Pierre Fabre, 1997. (Data on file).
A randomised, double-blind comparison of milnacipran and imipramine in the treatment of depression. Institut de Recherche Pierre Fabre, 1997. (Data on file).
Tignol J, Pujol-Domenech J, Chartres JP, et al. Double-blind study of the efficacy and safety of milnacipran (100 mg/day) and imipramine (100 mg/day) in elderly patents with major depressive episode. Acta Psychiatr Scand 1998; 97: 157–65
Lopez-Ibor J, Guelfi JD, Pletan Y, et al. Milnacipran and selective serotonin reuptake inhibitors in major depression. Int Clin Psychopharmacol 1996 Sep; 11 Suppl. 4: 41–6
Guelfi J-D, Ansseau M, Corruble E, et al. A double-blind comparison of the efficacy and safety of milnacipran and fluoxetine in severely depressed inpatients. Institut de Recherche Pierre Fabre, 1997. (Data on file).
Endo S, Miura S, Murasaki M, et al. Clinical evaluation of milnacipran hydrochloride, a new antidepressant for depression and depressive state. Phase III clinical trial with mianserin hydrochloride as a control drug [in Japanese]. Rinsho Hyoka 1995; 23(1): 39–64
Montgomery SA, Prost JF, Solles A, et al. Efficacy and tolerability of milnacipran: an overview. Int Clin Psychopharmacol 1996 Sep; 11 Suppl. 4: 47–51
Yamashita I, Onodera I, Ito K, et al. Clinical evaluation of TN-912 (milnacipran hydrochloride), a fourth generation antidepressant, in the late phase II study (dose finding study) [in Japanese]. Rinsho Iyaku 1994; 10(11): 2445–71
Tsutsui S, Nakano K, Tsuboi K, et al. Clinical effect of milnacipran hydrochloride (TN-912), a new antidepressant, in the field of psychosomatic medicine [in Japanese]. Rinsho Iyaku 1994; 10(11): 2473–88
Takahashi A, Murasaki M, Inami M, et al. Clinical utility of examination of milnacipran hydrochloride, a new antidepressant in the elderly [in Japanese]. Rinsho Iyaku 1995; 11 (5) Suppl. 3: 103–18
Pierre Fabre Medicament. Ixel 50mg antidepressant: SNRI serotonin and noradrenaline reuptake inhibitor. Boulogne: Pierre Fabre Medicament C.N.S. line, 1997. (Data on file).
Andrews JM, Nemeroff CB. Contemporary management of depression. Am J Med 1994 Dec 19; 97 Suppl. 6A: 24S–32S
Hirschfeld RMA. Schatzberg AF Long-term management of depression. Am J Med 1994 Dec 19; 97 Suppl. 6A: 33S–8S
McFarland BH. Cost-effectiveness considerations for managed care systems: treating depression in primary care. Am J Med 1994 Dec 19; 97 Suppl. 6A: 47S–58S
Leonard BE. Mechanisms of action of antidepressants. CNS Drugs 1995; 4 Suppl. 1: 1–12
Anderson IM, Tomenson BM. The efficacy of selective serotonin re-uptake inhibitors in depression: a meta-analysis of studies against tricyclic antidepressants. J Psychopharmacol 1994; 8(4): 238–49
Briley M, Prost JF, Moret C. Preclinical pharmacology of milnacipran. Int Clin Psychopharmacol 1996 Sep; 11 Suppl. 4: 10–4
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spencer, C.M., Wilde, M.I. Milnacipran. Drugs 56, 405–427 (1998). https://doi.org/10.2165/00003495-199856030-00010
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199856030-00010