Abstract
Purpose
We investigated the relationship between three-dimensional volumetric data of the metabolically active tumour volume assessed using [11C]-methionine positron emission tomography (MET-PET) and the area of gadolinium-diethylenetriaminepentaacetic acid (Gd-DTPA) enhancement assessed using magnetic resonance imaging (MRI) in patients with recurrent glioblastoma (GBM).
Material and methods
MET-PET and contrast-enhanced MRI with Gd-DTPA were performed in 12 uniformly pretreated patients with recurrent GBM. To calculate the volumes in cubic centimetres, a threshold-based volume-of-interest (VOI) analysis of the metabolically active tumour volume (MET uptake indexes of ≥1.3 and ≥1.5) and of the area of Gd-DTPA enhancement was performed after coregistration of all images.
Results
In all patients, the metabolically active tumour volume as shown using a MET uptake index of ≥1.3 was larger than the volume of Gd-DTPA enhancement (30.2 ± 22.4 vs. 13.7 ± 10.6 cm3; p = 0.04). Metabolically active tumour volumes as shown using MET uptake indexes of ≥1.3 and ≥1.5 and the volumes of Gd-DTPA enhancement showed a positive correlation (r = 0.76, p = 0.003, for an index of ≥1.3, and r = 0.74, p = 0.005, for an index of ≥1.5).
Conclusion
The present data suggest that in patients with recurrent GBM the metabolically active tumour volume may be substantially underestimated by Gd-DTPA enhancement. The findings support the notion that complementary information derived from MET uptake and Gd-DTPA enhancement may be helpful in developing individualized, patient-tailored therapy strategies in patients with recurrent GBM.
Similar content being viewed by others
Introduction
To date, the treatment of glioblastoma multiforme (GBM) remains a major challenge in clinical neurology because of its invasive characteristics. Infiltrative growing cells, which cannot be surgically extirpated in toto, are widely held to be responsible for recurrence of the tumour [1]. Currently, anatomical imaging using magnetic resonance imaging (MRI) is the most widely accepted method of determining the target for treatment. The area of gadolinium-diethylenetriaminepentaacetic acid (Gd-DTPA) enhancement is generally assumed to correspond well to the main mass of active tumour tissue. However, neuropathology has demonstrated that glioma cells are commonly found beyond the area of Gd-DTPA enhancement, particularly in GBM [2, 3].
Contrast enhancement depends on blood–brain barrier damage. Necrosis induced by therapy or occurring spontaneously during tumour progression may also show contrast enhancement and hence cannot be distinguished reliably from a solid tumour after therapy [4]. Therefore, imaging of the effectiveness of anticancer therapy by assessing the extent of MRI contrast enhancement is limited by the lack of distinction between tumour extent and contrast-enhancing necrosis. In addition, uptake of contrast agent may be substantially reduced by dexamethasone [5, 6] which is often necessary to reduce oedema in progressing tumours and thus modulates the applicability of contrast enhancement as an indicator of therapeutic efficiency. The fact that morphological imaging often does not adequately reflect the underlying tumour biology and its metabolic activity imposes a considerable demand to develop alternative biological markers for the therapeutic response.
The use of positron emission tomography (PET), an imaging technique providing metabolic data, may help improve diagnostic procedures in the management of malignant glioma. In PET studies, the radiotracer [11C]-methionine (MET) is the most widely used amino acid for brain tumour evaluation. MET-PET appears to be a valuable tool for defining the boundaries of malignant gliomas [7] and may thus help to refine individualized treatment strategies and the monitoring thereof.
Accumulation of MET is largely due to carrier-mediated transport, which is not altered by dexamethasone [8] and permits distinction between tumours and contrast-enhancing necrosis [9, 10]. MET is transported by the LAT1 amino acid transporter, which is highly expressed in cultured cells and malignant tumours [11, 12]. It undergoes complex metabolism and is incorporated into proteins; therefore, increased uptake may reflect the metabolic needs of brain tumours [13].
Previous PET studies in malignant gliomas have suggested that MET-PET allows an earlier and more accurate assessment of the tumour extent than contrast enhancement on CT and MRI alone [7, 14, 15]. For example, previous imaging data revealed that in patients with an untreated high-grade glioma the area of MET uptake as assessed using PET is larger than the area of Gd-DTPA enhancement delineated by MRI [16, 17]. Data assessment in these studies was, however, based upon a comparison of the maximal extent of the MET-PET uptake and Gd-DTPA enhancement, respectively, rather than a truly three-dimensional based volumetric assessment. A three-dimensional assessment of the active tumour volume may contribute, however, to improving the tailoring of a neurosurgical or radiotherapeutic intervention [18]. Additionally, complicated cranial neuronavigation procedures can be facilitated by three-dimensional information of the tumour extent [19].
We accordingly investigated the relationship between three-dimensional volumetric data of the metabolically active tumour volume and the area of Gd-DTPA enhancement in patients with recurrent GBM using a threshold-based volume of interest (VOI). We hypothesized that a volumetric assessment of MET-PET data may help to detect additional subareas of active tumour volume, over and above the information provided by Gd-DTPA enhancement alone.
Material and methods
We examined 12 patients (five women and seven men; mean age 58 ± 10 years, median 62 years, range 41–73 years) with recurrent glioblastoma who had been previously treated with a uniform standard therapy regimen [20] consisting of maximal neurosurgical resection (if possible), followed by concomitant radiation therapy with temozolomide (maximum radiation dose 60 Gy; 75 mg temozolomide per square metre of body surface area per day, 7 days per week from the first to the last day of radiotherapy), and initiation of adjuvant temozolomide chemotherapy (150–200 mg temozolomide per square metre of body-surface area over 5 days, repeated every 23 days; see Table 1). The diagnosis was confirmed histologically before initiating therapy. Due to a close localization of the tumour and eloquent brain areas or inoperability, in two patients neurosurgical resection could not be performed (patients 5 and 10). Based on temozolomide-related side effects (bone marrow depression), in two patients radiation therapy was performed alone (patients 7 and 11), and in one patient adjuvant temozolomide chemotherapy could not be continued (patient 8).
Recurrence of the glioblastoma was defined according to the Macdonald criteria (gadolinium enhancement or tumour enlargement ≥25%) with corresponding clinical deterioration [21]. The time to progression (TTP), defined as the time in months between initiation of the standard GBM therapy and tumour recurrence according to the Macdonald criteria, was determined.
MET-PET studies were performed in close temporal association with confirmation of the diagnosis “recurrent glioblastoma”. All patients gave written consent to participating in the MET-PET studies. PET studies were performed on an ECAT EXACT or ECAT EXACT HR scanner (Siemens/CTI, Knoxville, TN). Following a 10-min transmission scan, PET scans were performed after slow intravenous bolus injection of 740 MBq (20 mCi) of MET, synthesized according to the method of Berger et al. [22]. Tracer accumulation was recorded in three-dimensional mode over 60 min in 47 transaxial slices covering the entire brain. Summed activity from 20 to 60 min after tracer injection was used for image reconstruction. Images were reconstructed with Fourier rebinning and filtered back-projection with a ramp filter. Images were corrected for scatter, attenuation and random coincidences. Spatial resolution was 6 mm or better in all dimensions.
The MRI scan (1.5 T) was performed using a Gyroscan Intera scanner (Philips Medical Systems) and images were acquired using a standard head coil. Axial T1-weighted images were obtained from the second cervical vertebral body to the vertex. To provide a precise coregistration and accurate volume calculation, slice thickness was adjusted to 1 mm. After intravenous administration of Gd-DTPA (0.1 mmol/kg body weight), axial T1-weighted images were obtained using standard procedures.
PET data were evaluated by a region of interest (ROI) analysis. As described previously [8], a circular ROI (8 mm radius, surface area 201 mm2) was placed in the hottest area of the tumour (i.e. centred on the pixel with maximal activity). For reference, an identically sized circular ROI was placed on the unaffected corresponding contralateral cortex, or, if impossible because of the tumour location, on intact brain regions. The same procedure was performed with an approximately fourfold larger, irregularly shaped reference ROI (median surface area 838 ± 26 mm2) placed on the unaffected contralateral cortex to rule out systematic error, e.g. due to a partial volume effect in a smaller, identically sized reference ROI (Fig. 1). The tumour-to-contralateral mean activity ratio with both types of reference ROIs was calculated as an uptake index.
After coregistration of MR- and MET-PET images, a circular ROI (red circle, 8 mm radius, surface area 201 mm2) is placed in the hottest area of the tumour. For reference, an identical ROI (white circle, central image) and a larger irregularly shaped ROI (white irregular shape, bottom image, surface area 809 mm2 in this example) are placed on the unaffected contralateral cortex
Tumour volumes were measured by performing a three-dimensional thresholding based VOI analysis in all patients for MET-PET uptake and contrast-enhanced lesions on MRI, respectively, using the VINCI tool, developed in-house [23]. The threshold for increased MET uptake was set to ≥1.3 in the contiguous tumour region. In a previous study with mainly high-grade gliomas comparing the exact local MET uptake with histology of stereotaxically guided biopsies, a receiver operating characteristics analysis demonstrated a sensitivity of 87% and specificity of 89% for the detection of tumour tissue at a threshold of 1.3-fold MET uptake relative to normal brain tissue [7]. This threshold was confirmed in a further study using diffusion tensor imaging in comparison with MET uptake [24]. For comparison and to rule out false-positive results, the VOI analysis was also performed with a higher threshold (≥1.5). This threshold has been shown to provide the best separation between tumour and nontumour tissue in low-grade gliomas [8]. The threshold for positive contrast enhancement on MRI was determined by varying the value of the lower threshold to identify and separate the area of positive enhancement from the tissue with lower intensity.
The PET and MR images of each patient were coregistered with an accuracy of 2 mm or better using an automated procedure [25, 26] to ensure precise correspondence of ROI placement and to provide anatomical comparability of MET PET and MRI.
Descriptive statistics are provided as means and standard deviation and also as medians and range. The Spearman correlation test was used to calculate the correlation coefficient. Statistical analysis was performed using SigmaStat software (SigmaStat version 3.0, SPSS, Chicago, IL).
Results
The mean TTP after initiation of standard therapy was 12.2 ± 10.1 months (median TTP 8 months, range 4–40 months; see Table 2). No significant correlations between TTP and volumes of metabolically active tumour and volumes of Gd-DTPA enhancement, respectively, were observed.
By using a reference ROI of identical size, the mean MET uptake index was 2.04 ± 0.44 (median 2.01, range 1.50–2.95). There was no significant difference in the mean MET uptake index when using an approximately fourfold larger irregularly shaped reference ROI (mean index 2.04 ± 0.43, median 1.99, range 1.51–2.95; p>0.05, t-test; see Table 3). The median surface area of the larger irregularly shaped reference ROI was 838 ± 26 mm2 (in contrast, the surface area of the same-sized ROI was 201 mm2; see Fig. 1).
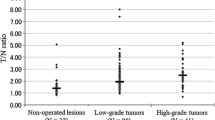
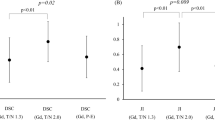
The metabolically active tumour volumes calculated using three-dimensional VOI analysis and a threshold of ≥1.3 or ≥1.5 were not significantly different between the two types of reference ROI (p>0.05, t-test; see Table 3). In contrast, the metabolically active tumour volumes were significantly larger using a threshold of ≥1.3 than when using a threshold of ≥1.5 for both types of reference ROI (p = 0.05, Mann-Whitney rank sum test; see Table 3, Fig. 3).
As expected in GBM, in all patients the tumours displayed areas of increased MET uptake and Gd-DTPA enhancement. The mean metabolically active tumour volume as shown by a MET uptake index of ≥1.3 was significantly higher than the mean volume of Gd-DTPA enhancement (30.2 ± 22.4 vs. 13.7 ± 10.6 cm3; p = 0.04, Mann-Whitney rank sum test; see Table 2, Fig. 2). In contrast, when using a MET uptake index of ≥1.5, the metabolically active tumour volume was not significantly different from the mean volume of Gd-DTPA enhancement (13.7 ± 9.5 vs. 13.7 ± 10.6 cm3; p>0.05, t-test; see Table 2).
Metabolically active tumour volumes as shown using MET uptake indexes of ≥1.3 and ≥1.5 and the volumes of Gd-DTPA enhancement showed a positive correlation (r = 0.76, p = 0.003, for an index of ≥1.3, and r = 0.74, p = 0.005, for an index of ≥1.5; Spearman correlation; see Fig. 3). In some patients, the location of the Gd-DTPA enhancement volume did not substantially differ from the location of the active tumour volume on MET-PET. In contrast, in other patients the volume of Gd-DTPA enhancement was not exclusively within the active tumour volume on MET-PET. On superimposed images, in these patients the volume of Gd-DTPA enhancement was often eccentric and partially located outside the active tumour volume on MET-PET (see Fig. 4). In these patients, especially those with a large Gd-DTPA enhancing volume, the location of Gd-DTPA enhancement did not correspond to MET uptake (see Table 4). The percentage of Gd-DTPA enhancing volume outside the area of the active tumour volume at a MET uptake threshold of ≥1.3 is shown for each patient in Table 4.
MR-, MET-PET and superimposed images of the active tumour volume (red) at a MET-uptake index threshold of ≥1.3 and volume of GTPA enhancement (white) in patient 1. Gd-DTPA enhancement is not always located exclusively within the subareas of the tumour positive on MET-PET. On superimposed pictures (bottom), Gd-DTPA enhancement is eccentric and located partially outside the active tumour volume
Discussion
The use of MET-PET, an imaging technique that provides metabolic information, may improve the ability of diagnostic procedures to determine the extent of malignant gliomas. However, to date an accurate three-dimensional comparison of the volumes of the metabolically active and contrast-enhanced subareas in patients with recurrent GBM is lacking. Previous PET studies of patients with untreated GBM have shown that the two-dimensionally assessed MET area corresponds well with the area of tumour extension and, moreover, GBM infiltration may extend well beyond the area of Gd-DTPA enhancement [16]. The aims of our study were (1) to compare three-dimensional metabolic and structural data of Gd-DTPA- and MET-positive tumour subareas, and (2) to provide evidence for its clinical significance in patients with recurrent GBM. The recent development of coregistration techniques for imaging data [23, 26] allows a more accurate integration of MET-PET metabolic data with MRI anatomical data, which may help to improve the clinical value of MET-PET scanning.
Our study shows that there are distinct differences in volumetric images of recurrent GBM between MET-PET and MRI, suggesting that in patients with recurrent GBM the metabolically active tumour volume extends considerably beyond the area of Gd-DTPA enhancement. These findings are in line with our hypothesis that a volumetric assessment of MET-PET data is able to detect subareas of active tumour volume in addition to those derived from Gd-DTPA enhancement alone.
In this study sample, TTP was within the range reported previously in mixed adult/elderly GBM patient populations [20]. The patients received standard therapy according to the EORTC 26981 study [20], except in two patients in whom the therapy was varied due to individual constraints, as detailed in Table 1. These individual constraints reflect the need for individual tailoring of therapy, e.g. to predict therapy failure as early as possible before clinical status deterioration and the appearance of side effects, i.e. bone marrow suppression, restrict the choice of rescue therapies.
A three-dimensional assessment of the active tumour volume may be helpful for more precise planning of a neurosurgical or radiotherapeutic intervention. Additionally, sophisticated cranial neuronavigation procedures could be facilitated by knowledge of three-dimensional information [19]. It has been shown previously, that volume reconstruction techniques may be used to increase the correlation between histological and in vivo tumour volume measurements in mouse models of human glioma [27]. Unlike previous data based upon a two-dimensional assessment of MET-PET imaging data [16], our noninvasive three-dimensional analysis of the volume of metabolically active tumour and the area of Gd-DTPA enhancement may provide further information as to the spatial configuration of the active tumour volume in relation to the volume of Gd-DTPA enhancement. Therefore, MET-PET- and MR-guided imaging with calculation of the metabolically active tumour volumes and the volumes of Gd-DTPA enhancement, respectively, may help improve the planning of specific, location-based tumour recurrence therapy strategies in patients with recurrent GBM (i.e. neurosurgical resection, focal radiotherapy).
Our data suggest that including MET-PET-derived three-dimensional information may help delineate more precisely the tumour extent and may thereby help improve neurosurgical resection. In various other recently presented studies, MET-PET data were successfully combined with MRI data to provide specific information for defining the target volume for radiosurgery and neuronavigation surgery in patients with brain tumours such as meningiomas and high-grade gliomas [18, 28, 29]. Our findings lend further support to the notion that MET-PET may provide complementary information to MRI, and may hence be helpful in improving future therapy strategies in patients with recurrent GBM. For example, in a recent study metabolic information helped planning of surgery using PET imaging-guided volumetric resection of high-grade gliomas [30]. It was demonstrated that complete resection according to PET tracer uptake in high-grade gliomas increases survival, whereas complete resection according to MRI contrast enhancement does not [30]. In this context, studies comparing the histology in different parts of the tumour and especially at the operative field margins according to local MET uptake and MRI enhancement are needed.
Concerning the methodological aspects of our study, variability in the measurement of the active tumour volume was exacerbated by using an inappropriately small circular ROI to determine the background reference level but this could be reduced by further assessment with an approximately fourfold larger, irregularly shaped reference ROI, which produced similar results. Furthermore, for calculation of the active tumour volumes we used different fixed thresholds (≥1.3 and ≥1.5) which both revealed significant correlations with the volume of Gd-DTPA enhancement. These observed significant correlations stress the validity of the method to calculate the active tumour volume. However, two outliers (patients 6 and 7; see Table 2, Fig. 3) with different active tumour volumes after data assessment using thresholds ≥1.3 and ≥1.5 were identified. This observation could be best explained by a relatively diffuse, widespread MET uptake pattern at the time of recurrence of GBM indicating highly malignant, infiltrative growing tumour biology in these patients.
Furthermore, the correlation between Gd-DTPA enhancement and MET uptake suggests that both phenomena are not independent but may be influenced by common underlying pathophysiological factors. Whereas in individual patients the location of Gd-DTPA enhancement volumes did not substantially differ from the location of the active tumour volume on MET-PET, in other patients Gd-DTPA enhancement volumes on superimposed images were often eccentric and partially located outside the active tumour volume on MET-PET. In these patients, especially those with large Gd-DTPA enhancing volumes, the location of Gd-DTPA enhancement did not match MET uptake. In these patients, MR and MET-PET imaging suggested necrotic tissue in the area of Gd-DTPA enhancement without MET uptake.
Due to the small number of patients in the current study, a larger study is needed to confirm the clinical usefulness of assessing the metabolically active tumour volume by MET-PET in patients with recurrent GBM. The current study, however, indicates the potential of MET-PET to more accurately assess recurrent GBM and opens new perspectives for the management of recurrent GBM. In the future, it seems likely that the complementary information obtained with multiple imaging modalities will lead to the most efficient delineation of the appropriate tumour volume.
References
Nazzaro JM, Neuwelt EA. The role of surgery in the management of supratentorial intermediate and high-grade astrocytomas in adults. J Neurosurg 1990;73:331–44.
Halperin EC, Bentel G, Heinz ER, Burger PC. Radiation therapy treatment planning in supratentorial glioblastoma multiforme: an analysis based on post mortem topographic anatomy with CT correlations. Int J Radiat Oncol Biol Phys 1989;17:1347–50.
Lunsford LD, Martinez AJ, Latchaw RE. Magnetic resonance imaging does not define tumor boundaries. Acta Radiol Suppl 1986;369:154–6.
Levivier M, Becerra A, De Witte O, Brotchi J, Goldman S. Radiation necrosis or recurrence. J Neurosurg 1996;84:148–9.
Cairncross JG, Macdonald DR, Pexman JH, Ives FJ. Steroid-induced CT changes in patients with recurrent malignant glioma. Neurology 1988;38:724–6.
Ostergaard L, Hochberg FH, Rabinov JD, Sorensen AG, Lev M, Kim L, et al. Early changes measured by magnetic resonance imaging in cerebral blood flow, blood volume, and blood-brain barrier permeability following dexamethasone treatment in patients with brain tumors. J Neurosurg 1999;90:300–5.
Kracht LW, Miletic H, Busch S, Jacobs AH, Voges J, Hoevels M, et al. Delineation of brain tumor extent with [11C]L-methionine positron emission tomography: local comparison with stereotactic histopathology. Clin Cancer Res 2004;10:7163–70.
Herholz K, Holzer T, Bauer B, Schroder R, Voges J, Ernestus RI, et al. 11C-methionine PET for differential diagnosis of low-grade gliomas. Neurology 1998;50:1316–22.
Reinhardt MJ, Kubota K, Yamada S, Iwata R, Yaegashi H. Assessment of cancer recurrence in residual tumors after fractionated radiotherapy: a comparison of fluorodeoxyglucose, L-methionine and thymidine. J Nucl Med 1997;38:280–7.
Sonoda Y, Kumabe T, Takahashi T, Shirane R, Yoshimoto T. Clinical usefulness of 11C-MET PET and 201T1 SPECT for differentiation of recurrent glioma from radiation necrosis. Neurol Med Chir (Tokyo) 1998;38:342–7; discussion 347–8.
Kim DK, Kanai Y, Choi HW, Tangtrongsup S, Chairoungdua A, Babu E, et al. Characterization of the system L amino acid transporter in T24 human bladder carcinoma cells. Biochim Biophys Acta 2002;1565:112–21.
Jager PL, Vaalburg W, Pruim J, de Vries EG, Langen KJ, Piers DA. Radiolabeled amino acids: basic aspects and clinical applications in oncology. J Nucl Med 2001;42:432–45.
Bustany P, Chatel M, Derlon JM, Darcel F, Sgouropoulos P, Soussaline F, et al. Brain tumor protein synthesis and histological grades: a study by positron emission tomography (PET) with C11-L-methionine. J Neurooncol 1986;3:397–404.
Bergstrom M, Collins VP, Ehrin E, Ericson K, Eriksson L, Greitz T, et al. Discrepancies in brain tumor extent as shown by computed tomography and positron emission tomography using [68Ga]EDTA, [11C]glucose, and [11C]methionine. J Comput Assist Tomogr 1983;7:1062–6.
Tovi M, Lilja A, Bergstrom M, Ericsson A, Bergstrom K, Hartman M. Delineation of gliomas with magnetic resonance imaging using Gd-DTPA in comparison with computed tomography and positron emission tomography. Acta Radiol 1990;31:417–29.
Miwa K, Shinoda J, Yano H, Okumura A, Iwama T, Nakashima T, et al. Discrepancy between lesion distributions on methionine PET and MR images in patients with glioblastoma multiforme: insight from a PET and MR fusion image study. J Neurol Neurosurg Psychiatry 2004;75:1457–62.
Pirotte B, Goldman S, Dewitte O, Massager N, Wikler D, Lefranc F, et al. Integrated positron emission tomography and magnetic resonance imaging-guided resection of brain tumors: a report of 103 consecutive procedures. J Neurosurg 2006;104:238–53.
Grosu AL, Weber WA, Riedel E, Jeremic B, Nieder C, Franz M, et al. L-(methyl-11C) methionine positron emission tomography for target delineation in resected high-grade gliomas before radiotherapy. Int J Radiat Oncol Biol Phys 2005;63:64–74.
Braun V, Dempf S, Weller R, Reske SN, Schachenmayr W, Richter HP. Cranial neuronavigation with direct integration of (11)C methionine positron emission tomography (PET) data – results of a pilot study in 32 surgical cases. Acta Neurochir (Wien) 2002;144:777–82; discussion 782.
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 2005;352:987–96.
Macdonald DR, Cascino TL, Schold SC Jr, Cairncross JG. Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 1990;8:1277–80.
Berger G, Maziere M, Knipper R, Prenant C, Comar D. Automated synthesis of 11C-labelled radiopharmaceuticals: imipramine, chlorpromazine, nicotine and methionine. Int J Appl Radiat Isot 1979;30:393–9.
Vollmar S, Hampl J, Kracht L, Herholz K. Integration of functional data (PET) into brain surgery planning and neuronavigation. In: Buzug TM, Holz D, Bongartz J, Kohl-Bareis M, Hartmann U, Weber S (editors) Advances in medical engineering. Berlin: Springer; 2007. p. 98–103.
Kinoshita M, Hashimoto N, Goto T, Yanagisawa T, Okita Y, Kagawa N, et al. Use of fractional anisotropy for determination of the cut-off value in 11C-methionine positron emission tomography for glioma. Neuroimage 2009;45:312–8.
Galldiks N, Kracht LW, Burghaus L, Thomas A, Jacobs AH, Heiss WD, et al. Use of 11C-methionine PET to monitor the effects of temozolomide chemotherapy in malignant gliomas. Eur J Nucl Med Mol Imaging 2006;33:516–24.
Cizek J, Herholz K, Vollmar S, Schrader R, Klein J, Heiss WD. Fast and robust registration of PET and MR images of human brain. Neuroimage 2004;22:434–42.
Schmidt KF, Ziu M, Schmidt NO, Vaghasia P, Cargioli TG, Doshi S, et al. Volume reconstruction techniques improve the correlation between histological and in vivo tumor volume measurements in mouse models of human gliomas. J Neurooncol 2004;68:207–15.
Grosu AL, Weber WA, Astner ST, Adam M, Krause BJ, Schwaiger M, et al. 11C-methionine PET improves the target volume delineation of meningiomas treated with stereotactic fractionated radiotherapy. Int J Radiat Oncol Biol Phys 2006;66:339–44.
Mahasittiwat P, Mizoe JE, Hasegawa A, Ishikawa H, Yoshikawa K, Mizuno H, et al. l-[METHYL-(11)C] methionine positron emission tomography for target delineation in malignant gliomas: impact on results of carbon ion radiotherapy. Int J Radiat Oncol Biol Phys 2008;70:515–22.
Pirotte BJ, Levivier M, Goldman S, Massager N, Wikler D, Dewitte O, et al. Positron emission tomography-guided volumetric resection of supratentorial high-grade gliomas: a survival analysis in 66 consecutive patients. Neurosurgery. 2009;64:471–81; discussion 481.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00259-010-1509-y
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Galldiks, N., Ullrich, R., Schroeter, M. et al. Volumetry of [11C]-methionine PET uptake and MRI contrast enhancement in patients with recurrent glioblastoma multiforme. Eur J Nucl Med Mol Imaging 37, 84–92 (2010). https://doi.org/10.1007/s00259-009-1219-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-009-1219-5