Abstract
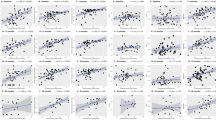
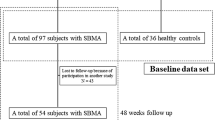
This study aimed to evaluate various metabolic parameters in patients with spinal and bulbar muscular atrophy (SBMA), to investigate the association between those indices and disease severity, and to explore the underlying molecular pathogenesis. We compared the degree of obesity, metabolic parameters, and blood pressure in 55 genetically confirmed SBMA patients against those in 483 age- and sex-matched healthy control. In SBMA patients, we investigated the correlation between these factors and motor functional indices. SBMA patients had lower body mass index, blood glucose, and Hemoglobin A1c, but higher blood pressure, homeostasis model assessment of insulin resistance (HOMA-IR, a marker of insulin resistance), total cholesterol, and adiponectin levels than the control subjects. There were no differences in visceral fat areas, high-density lipoprotein-cholesterol (HDL-C), or triglyceride levels in two groups. Revised amyotrophic lateral sclerosis functional rating scale (ALSFRS-R) correlated positively with HDL-C, but negatively with HOMA-IR. Through stepwise multiple regression analysis, we identified HOMA-IR as a significant metabolic determinant of ALSFRS-R. In biochemical analysis, we found that decreased expressions of insulin receptors, insulin receptor substrate-1 and insulin receptor-β, in autopsied muscles and fibroblasts of SBMA patients. This study demonstrates that SBMA patients have insulin resistance, which is associated with the disease severity. The expressions of insulin receptors are attenuated in the skeletal muscle of SBMA, providing a possible pathomechanism of metabolic alterations. These findings suggested that insulin resistance is a metabolic index reflecting disease severity and pathogenesis as well as a potential therapeutic target for SBMA.


Similar content being viewed by others
References
Katsuno M, Tanaka F, Adachi H et al (2012) Pathogenesis and therapy of spinal and bulbar muscular atrophy (SBMA). Prog Neurobiol 99:246–256
Giorgetti E, Lieberman AP (2016) Polyglutamine androgen receptor-mediated neuromuscular disease. Cell Mol Life Sci 73(21):3991–3999
La Spada AR, Wilson EM, Lubahn DB et al (1991) Androgen receptor gene mutations in X-linked spinal and bulbar muscular atrophy. Nature 352:77–79
Katsuno M, Adachi H, Kume A et al (2002) Testosterone reduction prevents phenotypic expression in a transgenic mouse model of spinal and bulbar muscular atrophy. Neuron 35:843–854
Adachi H, Katsuno M, Minamiyama M et al (2005) Widespread nuclear and cytoplasmic accumulation of mutant androgen receptor in SBMA patients. Brain 128:659–670
Sorarù G, D’Ascenzo C, Polo A et al (2008) Spinal and bulbar muscular atrophy: skeletal muscle pathology in male patients and heterozygous females. J Neurol Sci 264:100–105
Dejager S, Bry-Gauillard H, Bruckert E et al (2002) A comprehensive endocrine description of Kennedy’s disease revealing androgen insensitivity linked to CAG repeat length. J Clin Endocrinol Metab 87:3893–3901
Rhodes LE, Freeman BK, Auh S et al (2009) Clinical features of spinal and bulbar muscular atrophy. Brain 132:3242–3251
Hashizume A, Katsuno M, Banno H et al (2012) Longitudinal changes of outcome measures in spinal and bulbar muscular atrophy. Brain 135:2838–2848
Vagelatos NT, Eslick GD (2013) Type 2 diabetes as a risk factor for Alzheimer’s disease: the confounders, interactions, and neuropathology associated with this relationship. Epidemiol Rev 35:152–160
Xu Q, Park Y, Huang X et al (2011) Diabetes and risk of Parkinson’s disease. Diabetes Care 34:910–915
Dupuis L, Corcia P, Fergani A et al (2008) Dyslipidemia is a protective factor in amyotrophic lateral sclerosis. Neurology 70:1004–1009
Kioumourtzoglou MA, Rotem RS, Seals RM et al (2015) Diabetes mellitus, obesity, and diagnosis of amyotrophic lateral sclerosis: a population-based study. JAMA Neurol 72:905–911
Shimojo D, Onodera K, Doi-Torii Y et al (2015) Rapid, efficient, and simple motor neuron differentiation from human pluripotent stem cells. Mol Brain 8:79
Hijikata H, Katsuno M, Suzuki K et al (2016) Impaired muscle uptake of creatine in spinal and bulbar muscular atrophy. Ann Clin Transl Neurol 3:537–546
Nakatsuji H, Kishida K, Kitamura T et al (2010) Dysregulation of glucose, insulin, triglyceride, blood pressure, and oxidative stress after an oral glucose tolerance test in men with abdominal obesity. Metabolism 59:520–526
Matthews DR, Hosker JP, Rudenski AS et al (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Querin G, Bertolin C, Da Re E et al (2016) Non-neural phenotype of spinal and bulbar muscular atrophy: results from a large cohort of Italian patients. J Neurol Neurosurg Psychiatry 87:810–816
Iida M, Katsuno M, Nakatsuji H et al (2015) Pioglitazone suppresses neuronal and muscular degeneration caused by polyglutamine-expanded androgen receptors. Hum Mol Genet 24:314–329
Yu IC, Lin HY, Sparks JD et al (2014) Androgen receptor roles in insulin resistance and obesity in males: the linkage of androgen-deprivation therapy to metabolic syndrome. Diabetes 63:3180–3188
Maeda N, Shimomura I, Kishida K et al (2002) Diet-induced insulin resistance in mice lacking adiponectin/ACRP30. Nat Med 8:731–737
Cortes CJ, Ling SC, Guo LT et al (2014) Muscle expression of mutant androgen receptor accounts for systemic and motor neuron disease phenotypes in spinal and bulbar muscular atrophy. Neuron 82:295–307
Palazzolo I, Stack C, Kong L et al (2009) Overexpression of IGF-1 in muscle attenuates disease in a mouse model of spinal and bulbar muscular atrophy. Neuron 63:316–328
Srikanthan P, Hevener AL, Karlamangla AS (2010) Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: findings from the National Health and Nutrition Examination Survey III. PLoS One 5:e10805
Wijngaarden MA, van der Zon GC, van Dijk KW et al (2013) Effects of prolonged fasting on AMPK signaling, gene expression, and mitochondrial respiratory chain content in skeletal muscle from lean and obese individuals. Am J Physiol Endocrinol Metab 304:E1012–E1021
Swan JW, Anker SD, Walton C et al (1997) Insulin resistance in chronic heart failure: relation to severity and etiology of heart failure. J Am Coll Cardiol 30:527–532
Ouchi N, Parker JL, Lugus JJ et al (2011) Adipokines in inflammation and metabolic disease. Nat Rev Immunol 11:85–97
Nishizawa H, Shimomura I, Kishida K et al (2002) Androgens decrease plasma adiponectin, an insulin-sensitizing adipocyte-derived protein. Diabetes 51:2734–2741
Craft S, Watson GS (2004) Insulin and neurodegenerative disease: shared and specific mechanisms. Lancet Neurol 3:169–178
Santiago JA, Potashkin JA (2013) Shared dysregulated pathways lead to Parkinson’s disease and diabetes. Trends Mol Med 19:176–186
Lalić NM, Marić J, Svetel M et al (2008) Glucose homeostasis in Huntington disease: abnormalities in insulin sensitivity and early-phase insulin secretion. Arch Neurol 65:476–480
Lalić NM, Dragasević N, Stefanova E et al (2010) Impaired insulin sensitivity and secretion in normoglycemic patients with spinocerebellar ataxia type 1. Mov Disord 25:1976–1980
Yu Z, Wang AM, Adachi H et al (2011) Macroautophagy is regulated by the UPR-mediator CHOP and accentuates the phenotype of SBMA mice. PLoS Genet 7:e1002321
Navarro G, Allard C, Xu W et al (2015) The role of androgens in metabolism, obesity, and diabetes in males and females. Obesity (Silver Spring) 23:713–719
Chang PY, Benecke H, Le Marchand-Brustel Y et al (1994) Expression of a dominant-negative mutant human insulin receptor in the muscle of transgenic mice. J Biol Chem 269:16034–16040
Hilder TL, Tou JC, Grindeland RE et al (2003) Phosphorylation of insulin receptor substrate-1 serine 307 correlates with JNK activity in atrophic skeletal muscle. FEBS Lett 553:63–67
Minamiyama M, Katsuno M, Adachi H et al (2012) Naratriptan mitigates CGRP1-associated motor neuron degeneration caused by an expanded polyglutamine repeat tract. Nat Med 18:1531–1538
Lee CG, Boyko EJ, Strotmeyer ES et al (2011) Association between insulin resistance and lean mass loss and fat mass gain in older men without diabetes mellitus. J Am Geriatr Soc 59:1217–1224
Kalonia H, Kumar P, Kumar A (2010) Pioglitazone ameliorates behavioral, biochemical and cellular alterations in quinolinic acid induced neurotoxicity: possible role of peroxisome proliferator activated receptor-Upsilon (PPARUpsilon) in Huntington’s disease. Pharmacol Biochem Behav 96:115–124
Dehmer T, Heneka MT, Sastre M et al (2004) Protection by pioglitazone in the MPTP model of Parkinson’s disease correlates with I kappa B alpha induction and block of NF kappa B and iNOS activation. J Neurochem 88:494–501
Kiaei M, Kipiani K, Chen J et al (2005) Peroxisome proliferator-activated receptor-gamma agonist extends survival in transgenic mouse model of amyotrophic lateral sclerosis. Exp Neurol 191:331–336
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work was supported by the Grant-in-Aids (KAKENHI) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (Nos. 26293206, 26670440, 2667043, 15K15337, and 16K15480) and a Grant from the Japan Agency for Medical Research and Development (AMED) (No. 15ek0109025).
Conflicts of interest
Drs. Nakatsuji, Araki, Hashizume, Hijikata, Yamada, Inagaki, Suzuki, Banno, Suga, Ohyama, Nakagawa, and Shimomura report no disclosures.
Dr. Okada is supported by KAKENHI Grants from MEXT/JSPS, Japan (Nos. 25640038, 25110730, 15H04278, and 15H01568), a Grant from the Japan Agency for Medical Research and Development (AMED) (No. 15ek0109025, 15ek0109048, and 15ek0109165), and Grants from the Ministry of Welfare, Health, and Labor of Japan.
Dr. Kishida is supported in part by a Grant-in-Aid for Scientific Research on Innovative Areas (Research in a proposed research area) “Molecular Basis and Disorders of Control of Appetite and Fat Accumulation” (No. 22126008).
Dr. Funahashi is supported in part by a Grant-in-Aid for Scientific Research on Innovative Areas (Research in a proposed research area) “Molecular Basis and Disorders of Control of Appetite and Fat Accumulation” (No. 22126008). He is a member of the “Department of Metabolism and Atherosclerosis”, a sponsored course endowed by Kowa Co. Ltd. The company has a scientific officer who oversees the program.
Dr. Okano is a founder scientist of SanBio Co. Ltd and K Pharma Co. Ltd. He is supported by the Program for Intractable Disease Research Utilizing Disease-specific iPS Cells funded by the Japan Science and Technology Agency (JST)/Japan Agency for Medical Research and Development (AMED).
Dr. Katsuno is supported by KAKENHI Grants from MEXT/JSPS, Japan (Nos. 26293206, 26670440, 2667043, 15K15337, and 16K15480) and a Grant from the Japan Agency for Medical Research and Development (AMED) (No. 15ek0109025 and 15ek0109165).
Dr. Sobue serves as a scientific advisory board member for the Kanae Science Foundation for the Promotion of Medical Science, Naito Science Foundation; an advisory board member of Brain; and an editorial board member of Degenerative Neurological and Neuromuscular Disease, the Journal of Neurology, and Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. He is supported by KAKENHI Grants from MEXT/JSPS, Japan (Nos. 26117001); Grants from the Japan Science and Technology Agency; Grants from the Japan Agency for Medical Research and Development (AMED) (Nos. 15ek0109025, 15ek0109048, and 15ek0109165); and Grants from the Ministry of Welfare, Health, and Labor of Japan.
Ethical standards
This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nakatsuji, H., Araki, A., Hashizume, A. et al. Correlation of insulin resistance and motor function in spinal and bulbar muscular atrophy. J Neurol 264, 839–847 (2017). https://doi.org/10.1007/s00415-017-8405-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-017-8405-3