Abstract
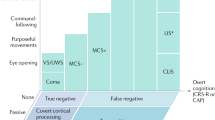
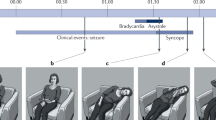
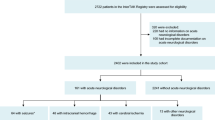
Episodes of transient loss of consciousness (TLOC) events pose diagnostic difficulties, as the causes are diverse, carry vastly different risks, and span various specialties. An inconsistent terminology contributes to the confusion. Here, we present a classification scheme for TLOC, based on ongoing multidisciplinary efforts including those of the Task Force on Syncope of the European Society of Cardiology. We also discuss the pathophysiology of TLOC and the key clinical features that aid diagnosis. TLOC is defined as an apparent loss of consciousness with an abrupt onset, a short duration, and a spontaneous and complete recovery. Syncope is defined as TLOC due to cerebral hypoperfusion, and is divided into reflex syncope (synonymous with neurally mediated syncope), syncope due to orthostatic hypotension, and cardiac syncope (arrhythmic or associated with structural cardiac disease). The other major groups of TLOC are generalized epileptic seizures, functional TLOC (psychogenic TLOC mimicking either epilepsy or syncope), and a further group of miscellaneous disorders. The management of patients who experience TLOC requires the recognition of the defining features of each of the major groups, and cooperation between different clinical specialties.
Key Points
-
Transient loss of consciousness (TLOC) is an apparent loss of consciousness with an abrupt onset, short duration, and spontaneous and complete recovery
-
TLOC is a distinct diagnostic group comprising syncope, generalized epileptic seizures, functional TLOC and a group of rare causes
-
Syncope is divided into reflex syncope, syncope due to orthostatic hypotension and cardiac syncope
-
Reflex syncope is by far the most common form of TLOC and might affect up to 40% of the population
-
Diagnosis of TLOC requires an understanding of key clues, pathophysiology and underlying epidemiological patterns, and entails a multidisciplinary approach
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Landau, W. M. & Nelson, D. A. Clinical neuromythology XV. Feinting science: neurocardiogenic syncope and collateral vasovagal confusion. Neurology 46, 609–618 (1996).
Josephson, C. B., Rahey, S. & Sadler, R. M. Neurocardiogenic syncope: frequency and consequences of its misdiagnosis as epilepsy. Can. J. Neurol. Sci. 34, 221–224 (2007).
Carreño, M. Recognition of nonepileptic events. Semin. Neurol. 28, 297–304 (2008).
Chowdhury, F. A., Nashef, L. & Elwes, R. D. Misdiagnosis in epilepsy: a review and recognition of diagnostic uncertainty. Eur. J. Neurol. 15, 1034–1042 (2008).
Colman, N. et al. Epidemiology of reflex syncope. Clin. Auton. Res. 14 (Suppl. 1), 9–17 (2004).
Ganzeboom, K. S., Colman, N., Reitsma, J. B., Shen, W. K. & Wieling, W. Prevalence and triggers of syncope in medical students. Am. J. Cardiol. 15, 1006–1008 (2003).
Ganzeboom, K. S. et al. Lifetime cumulative incidence of syncope in the general population: a study of 549 Dutch subjects aged 35–60 years. J. Cardiovasc. Electrophysiol. 17, 1172–1176 (2006).
van Dijk, J. G. Explaining syncope: faints need not confuse. Europace 7, 392–395 (2005).
van Dijk, J. G. & Fitzpatrick, A. P. What is syncope and what is not syncope: the importance of definitions. In The Evaluation and Treatment of Syncope. A Handbook for Clinical Practice 2nd edn (Eds Benditt, D. G., Blanc, J. J., Brignole, M. & Sutton, R.) 10–15 (Wiley-Blackwell, Oxford 2006).
Thijs, R. D., Granneman, E., Wieling, W. & van Dijk, J. G. Terms in use for transient loss of consciousness in the emergency ward; an inventory [Dutch]. Ned. Tijdschr. Geneeskd. 149, 1625–1630 (2005).
Thijs, R. D. et al. Unconscious confusion—a literature search for definitions of syncope and related disorders. Clin. Auton. Res. 15, 35–39 (2005).
Brignole, M. et al. Guidelines on management (diagnosis and treatment) of syncope. Eur. Heart J. 22, 1256–1306 (2001).
The Task Force on Syncope, European Society of Cardiology. Guidelines on management (diagnosis and treatment) of syncope—update 2004. Europace 6, 467–537 (2004).
Thijs, R. D., Wieling, W., Kaufmann, H. & van Dijk, J. G. Defining and classifying syncope. Clin. Auton. Res. 14 (Suppl. 1), 4–8 (2004).
Jhanjee, R., van Dijk, J. G., Sakaguchi, S. & Benditt, D. G. Syncope in adults: terminology, classification, and diagnostic strategy. Pacing Clin. Electrophysiol. 29, 1160–1169 (2006).
Posner, J. B., Saper, C. B., Schiff, N. & Plum, F. Plum and Posner's Diagnosis of Stupor and Coma 4th edn (Oxford University Press, New York, 2007).
Bloem, R., Overeem, S. & van Dijk, J. G. Syncopal falls, drop attacks and their mimics. In Clinical Disorders of Balance, Posture and Gait 2nd edn (Eds Bronstein, A. M., Brandt, T., Woollacott, M. J. & Nutt, J. G.) 287–316 (Hodder Arnold, London, 2004).
Rossen, R., Kabat, H. & Anderson, J. P. Acute arrest of cerebral circulation in man. Arch. Neurol. Psychiatry 50, 510–528 (1943).
Lempert, T., Bauer, M. & Schmidt, D. Syncope: a videometric analysis of 56 episodes of transient cerebral hypoxia. Ann. Neurol. 36, 233–237 (1994).
Lempert, T. & von Brevern, M. The eye movements of syncope. Neurology 46, 1086–1088 (1996).
Stephenson, J. B. P. Fits and Faints (MacKeith Press, Oxford, 1990).
Lin, J. T., Ziegler, D. K., Lai, C. W. & Bayer, W. Convulsive syncope in blood donors. Ann. Neurol. 11, 525–528 (1982).
Newman, B. H. & Graves, S. A study of 178 consecutive vasovagal syncopal reactions from the perspective of safety. Transfusion 41, 1475–1479 (2001).
Hoefnagels, W. A., Padberg, G. W., Overweg, J., van der Velde, E. A. & Roos, R. A. Transient loss of consciousness: the value of the history for distinguishing seizure from syncope. J. Neurol. 238, 39–43 (1991).
Romme, J. J. et al. Influence of age and gender on the occurrence and presentation of reflex syncope. Clin. Auton. Res. 18, 127–133 (2008).
Benbadis, S. R., Wolgamuth, B. R., Goren, H., Brener, S. & Fouad-Tarazi, F. Value of tongue biting in the diagnosis of seizures. Arch. Intern. Med. 155, 2346–2349 (1995).
Serletis, A., Rose, S., Sheldon, A. G. & Sheldon, R. S. Vasovagal syncope in medical students and their first-degree relatives. Eur. Heart J. 27, 1965–1970 (2006).
Olde Nordkamp, L. R., Wieling, W., Zwinderman, A. H., Wilde, A. A. & van Dijk, N. Genetic aspects of vasovagal syncope: a systematic review of current evidence. Europace 11, 414–420 (2009).
Sheldon, R. S. et al. Age of first faint in patients with vasovagal syncope. J. Cardiovasc. Electrophysiol. 17, 49–54 (2006).
Alboni, P., Alboni, M. & Bertorelle, G. The origin of vasovagal syncope: to protect the heart or to escape predation? Clin. Auton. Res. 18, 170–178 (2008).
van Dijk, J. G. Fainting in animals. Clin. Auton. Res. 13, 247–255 (2003).
van Dijk, J. G. & Sheldon, R. Is there any point to vasovagal syncope? Clin. Auton. Res. 18, 167–169 (2008).
Hainsworth, R. Pathophysiology of syncope. Clin. Auton. Res. 14 (Suppl. 1), 18–24 (2004).
Verheyden, B. et al. Steep fall in cardiac output is main determinant of hypotension during drug-free and nitroglycerine-induced orthostatic vasovagal syncope. Heart Rhythm 5, 1695–1701 (2008).
Gracie, J., Newton, J. L., Norton, M., Baker, C. & Freeston, M. The role of psychological factors in response to treatment in neurocardiogenic (vaovagal) syncope. Europace 8, 636–643 (2006).
Fucà, G. et al. The venous system is the main determinant of hypotension in patients with vasovagal syncope. Europace 8, 839–845 (2006).
Verheyden, B. et al. Impact of age on the vasovagal response provoked by sublingual nitroglycerine in routine tilt testing. Clin. Sci. (Lond.) 113, 329–337 (2007).
Krediet, C. T., Wilde, A. A., Wieling, W. & Halliwill, J. R. Exercise related syncope, when it's not the heart. Clin. Auton. Res. 14 (Suppl. 1), 25–36 (2004).
Kerr, S. R., Pearce, M. S., Brayne, C., Davis, R. J. & Kenny, R. A. Carotid sinus hypersensitivity in asymptomatic older persons: implications for diagnosis of syncope and falls. Arch. Intern. Med. 166, 515–520 (2006).
Parry, S. W., Steen, N., Bexton, R., Tynan, M. & Kenny, R. A. Pacing in elderly recurrent fallers with carotid sinus hypersensitivity: a randomised, double-blind, placebo controlled cross-over trial. Heart 95, 405–409 (2009).
van Dijk, N. et al. Clinical factors associated with quality of life in patients with transient loss of consciousness. J. Cardiovasc. Electrophysiol. 17, 998–1003 (2006).
van Dijk, N. et al. Quality of life within one year following presentation after transient loss of consciousness. Am. J. Cardiol. 100, 672–676 (2007).
Ross, R., Parry, S., Norton, M. & Newton, J. L. Self-reported symptom burden; outcome in 418 patients from the Newcastle Vasovagal (Neurocardiogenic) cohort. QJM 101, 127–135 (2008).
Ammirati, F. et al. Management of syncope: clinical and economic impact of a Syncope Unit. Europace 10, 471–476 (2008).
Kaufmann, H. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure and multiple system atrophy. Clin. Auton. Res. 6, 125–126 (1996).
Low, P. A. & Singer, W. Management of neurogenic orthostatic hypotension: an update. Lancet Neurol. 7, 451–458 (2008).
Lahrmann, H. et al. EFNS guidelines on the diagnosis and management of orthostatic hypotension. Eur. J. Neurol. 13, 930–936 (2006).
Robertson, D. The pathophysiology and diagnosis of orthostatic hypotension. Clin. Auton. Res. 18 (Suppl. 1), 2–7 (2008).
Naschitz, J. E. & Rosner, I. Orthostatic hypotension: framework of the syndrome. Postgrad. Med. J. 83, 568–574 (2007).
Freeman, R. Clinical Practice. Neurogenic orthostatic hypotension. N. Engl. J. Med. 358, 615–624 (2008).
Wieling, W. & Schatz, I. The consensus statement on the definition of orthostatic hypotension. A revisit after 13 years. J. Hypertension 27, 935–938 (2009).
Gehrking, J. A. et al. What is the minimum duration of head-up tilt necessary to detect orthostatic hypotension? Clin. Auton. Res. 15, 71–75 (2005).
Gibbons, C. H. & Freeman, R. Delayed orthostatic hypotension: a frequent cause of orthostatic intolerance. Neurology 67, 28–32 (2006).
Bleasdale-Barr, K. M. & Mathias, C. J. Neck and other muscle pains in autonomic failure: their association with orthostatic hypotension. J. R. Soc. Med. 91, 355–359 (1998).
Smith, G. D., Watson, L. P., Pavitt, D. V. & Mathias, C. J. Abnormal cardiovascular and catecholamine responses to supine exercise in human subjects with sympathetic dysfunction. J. Physiol. 484, 255–265 (1995).
Smith, G. D. & Mathias, C. J. Postural hypotension enhanced by exercise in patients with chronic autonomic failure. QJM 88, 251–256 (1995).
Wieling, W., Krediet, C. T., van Dijk, N., Linzer, M. & Tschakovsky, M. E. Initial orthostatic hypotension: review of a forgotten condition. Clin. Sci. (Lond.) 112, 157–165 (2007).
Podoleanu, C. et al. Lower limb and abdominal compression bandages prevent progressive orthostatic hypotension in elderly persons: a randomized single-blind controlled study. J. Am. Coll. Cardiol. 48, 1425–1432 (2006).
Soteriades, E. S. et al. Incidence and prognosis of syncope. N. Engl. J. Med. 347, 878–885 (2002).
Kannankeril, P. J. & Roden, D. M. Drug-induced long QT and torsade de pointes: recent advances. Curr. Opin. Cardiol. 22, 39–43 (2007).
Meyer, J. S., Mehdirad, A., Salem, B. I., Kulikowska, A. & Kulikowski, P. Sudden arrhythmia death syndrome: importance of the long QT syndrome. Am. Fam. Physician 68, 483–488 (2003).
Vohra, J. The long QT syndrome. Heart Lung Circ. 16 (Suppl. 3), S5–S12 (2007).
Alboni, P. et al. Diagnostic value of history in patients with syncope with or without heart disease. J. Am. Coll. Cardiol. 37, 1921–1928 (2001).
Sheldon, R. et al. Diagnostic criteria for vasovagal syncope based on a quantitative history. Eur. Heart J. 27, 344–350 (2006).
Wieling, W., Krediet, C. T. & Wilde, A. A. Flush after syncope: not always an arrhythmia. J. Cardiovasc. Electrophysiol. 17, 804–805 (2006).
So, N. K. Atonic phenomena and partial seizures. A reappraisal. Adv. Neurol. 67, 29–39 (1995).
Trenité, D. G. Photosensitivity, visually sensitive seizures and epilepsies. Epilepsy Res. 70 (Suppl. 1), S269–S279 (2006).
Bakker, M. J., van Dijk, J. G., van den Maagdenberg, A. M. & Tijssen, M. A. Startle syndromes. Lancet Neurol. 5, 513–524 (2006).
Tibussek, D., Wohlrab, G., Boltshauser, E. & Schmitt, B. Proven startle-provoked epileptic seizures in childhood: semiologic and electrophysiologic variability. Epilepsia 47, 1050–1058 (2006).
Levine, E. et al. Congenital long QT syndrome: considerations for primary care physicians. Cleve. Clin. J. Med. 75, 591–600 (2008).
van Donselaar, C. A., Geerts, A. T. & Schimsheimer, R. J. Usefulness of an aura for classification of a first generalized seizure. Epilepsia 31, 529–535 (1990).
Colman, N. et al. Diagnostic value of history taking in reflex syncope. Clin. Auton. Res. 14 (Suppl. 1), 37–44 (2004).
Sheldon, R. et al. Historical criteria that distinguish syncope from seizures. J. Am. Coll. Cardiol. 40, 142–148 (2002).
Ghearing, G. R., Munger, T. M., Jaffe, A. S., Benarroch, E. E. & Britton, J. W. Clinical clues for detecting ictal asystole. Clin. Auton. Res. 17, 221–226 (2007).
Horrocks, I. A., Nechay, A., Stephenson, J. B. & Zuberi, S. M. Anoxic-epileptic seizures: observational study of epileptic seizures induced by syncopes. Arch. Dis. Child. 90, 1283–1287 (2005).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR Fourth Edition (Text Revision) 4th edn (American Psychiatric Publishing, Inc., Arlington, VA, 2000).
Kroenke, K., Sharpe, M. & Sykes, R. Revising the classification of somatoform disorders: key questions and preliminary recommendations. Psychosomatics 48, 277–285 (2007).
Kroenke, K. & Rosmalen, J. G. Symptoms, syndromes, and the value of psychiatric diagnostics in patients who have functional somatic disorders. Med. Clin. North Am. 90, 603–626 (2006).
Reuber, M., Howlet, S., Khan, A. & Grünewald, R. A. Non-epileptic seizures and other functional neurological symptoms: predisposing, precipitating, and perpetuating factors. Psychosomatics 48, 230–238 (2007).
Strassnig, M., Stowell, K. R., First, M. B. & Pincus, H. A. General medical and psychiatric perspectives on somatoform disorders: separated by an uncommon language. Curr. Opin. Psychiatry 19, 194–200 (2006).
Benbadis, S. R. The problem of psychogenic symptoms: is the psychiatric community in denial? Epilepsy Behav. 6, 9–14 (2005).
Reuber, M., Mitchell, A. J., Howlett, S. J., Crimlisk, H. L. & Grünewald, R. A. Functional symptoms in neurology: questions and answers. J. Neurol. Neurosurg. Psychiatry 76, 307–314 (2005).
Stone, J. et al. What should we call pseudoseizures? The patient's perspective. Seizure 12, 568–572 (2003).
Oliva, M. et al. The diagnostic value of oral lacerations and incontinence during convulsive 'seizures'. Epilepsia 49, 962–967 (2008).
LaFrance, W. C. Jr. Psychogenic nonepileptic seizures. Curr. Opin. Neurol. 21, 195–201 (2008).
Chung, S. S., Gerber, P. & Kirlin, K. A. Ictal eye closure is a reliable indicator for psychogenic nonepileptic seizures. Neurology 66, 1730–1731 (2006).
Syed, T. U. et al. Do observer and self-reports of ictal eye closure predict psychogenic nonepileptic seizures? Epilepsia 49, 898–904 (2008).
Thijs, R. D., Wagenaar, W. A., Middelkoop, H. A., Wieling, W. & van Dijk, J. G. Transient loss of consciousness through the eyes of a witness. Neurology 71, 1713–1718 (2008).
Zaidi, A., Crampton, S., Clough, P., Fitzpatrick, A. & Scheepers, B. Head-up tilting is a useful provocative test for psychogenic non-epileptic seizures. Seizure 8, 353–355 (1999).
Ribaï, P., Tugendhaft, P. & Legros, B. Usefulness of prolonged video-EEG monitoring and provocative procedure with saline injection for the diagnosis of nonepileptic seizures of psychogenic origin. J. Neurol. 253, 328–332 (2006).
Petersen, M. E., Williams, T. R. & Sutton, R. Psychogenic syncope diagnosed by prolonged head-up tilt testing. QJM 88, 209–213 (1995).
van Dijk, N. et al. High diagnostic yield and accuracy of history, physical examination, and ECG in patients with transient loss of consciousness in FAST: the Fainting Assessment study. J. Cardiovasc. Electrophysiol. 19, 48–55 (2008).
Benbadis, S. R. & Chichkova, R. Psychogenic pseudosyncope: an underestimated and provable diagnosis. Epilepsy Behav. 9, 106–110 (2006).
Savitz, S. I. & Caplan, L. R. Vertebrobasilar disease. N. Engl. J. Med. 352, 2618–2626 (2005).
Hennerici, M., Klemm, C. & Rautenberg, W. The subclavian steal phenomenon: a common vascular disorder with rare neurologic deficits. Neurology 38, 669–673 (1988).
Taylor, C. L., Selman, W. R. & Ratchson, R. A. Steal affecting the central nervous system. Neurosurgery 50, 679–689 (2002).
Stark, R. J. & Wodak, J. Primary orthostatic cerebral ischaemia. J. Neurol. Neurosurg. Psychiatry 46, 883–891 (1983).
American Academy of Sleep Medicine. The International Classification of Sleep Disorders. Diagnostic and Coding Manual 2nd edn (American Academy of Sleep Medicine, Westchester, Illinois, 2005).
Overeem, S., Mignot, E., van Dijk, J. G. & Lammers, G. J. Narcolepsy: clinical features, new pathophysiological insights, and future perspectives. J. Clin. Neurophysiol. 18, 78–105 (2001).
Macleod, S., Ferrie, C. & Zuberi, S. M. Symptoms of narcolepsy in children misinterpreted as epilepsy. Epileptic Disord. 7, 13–17 (2005).
Zeman, A., Douglas, N. & Aylward, R. Lesson of the week: narcolepsy mistaken for epilepsy. BMJ 322, 216–218 (2001).
Calabrò, R. S. et al. Status cataplecticus misdiagnosed as recurrent syncope. Neurol. Sci. 28, 336–338 (2007).
Stevens, D. L. & Matthews, W. B. Cryptogenic drop attacks: an affliction of women. BMJ 1, 439–442 (1973).
Friedman, M. J., Mull, C. C., Sharieff, G. Q. & Tsarouhas, N. Prolonged QT syndrome in children: an uncommon but potentially fatal entity. J. Emerg. Med. 24, 173–179 (2003).
Kotsopoulos, I. et al. Incidence of epilepsy and predictive factors of epileptic and non-epileptic seizures. Seizure 14, 175–182 (2005).
Olafsson, E. et al. Incidence of unprovoked seizures and epilepsy in Iceland and assessment of the epilepsy syndrome classification: a prospective study. Lancet Neurol. 4, 627–634 (2005).
Sillanpää, M., Kälviäinen, R., Klaukka, T., Helenius, H. & Shinnar, S. Temporal changes in the incidence of epilepsy in Finland: nationwide study. Epilepsy Res. 71, 206–215 (2006).
Olde Noordkamp, L. R. et al. Syncope prevalence in the ED compared to that in the genral practice and population: a strong selection process. Am. J. Emergency Med. 27, 271–279 (2009).
Martikainen, K. et al. Transient loss of consciousness with and without injuries: where to treat these patients? Eur. J. Gen. Pract. 9, 91–95 (2003).
Martikainen, K. et al. Transient loss of consciousness as reason for admission to primary health care emergency room. Scand. J. Prim. Health Care 21, 61–64 (2003).
Bartoletti, A. et al. Physical injuries caused by a transient loss of consciousness: main clinical characteristics of patients and diagnostic contribution of carotid sinus massage. Eur. Heart J. 29, 618–624 (2008).
Gilbert, D. L., Sthuraman, G., Kotagal, U. & Buncher, R. Meta-analysis of EEG test performance shows wide variation among studies. Neurology 60, 564–570 (2002).
van Donselaar, C. A., Stroink, H., Arts, W. F. & Dutch Study Group of Epilepsy in Childhood. How confident are we of the diagnosis of epilepsy? Epilepsia 47 (Suppl. 1), 9–13 (2006).
Acknowledgements
The authors are indebted to Ley Sander and Wil Hoefnagels for helpful comments on the manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
van Dijk, J., Thijs, R., Benditt, D. et al. A guide to disorders causing transient loss of consciousness: focus on syncope. Nat Rev Neurol 5, 438–448 (2009). https://doi.org/10.1038/nrneurol.2009.99
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2009.99
This article is cited by
-
Vagal sensory neurons mediate the Bezold–Jarisch reflex and induce syncope
Nature (2023)
-
Calgary score and modified calgary score in the differential diagnosis between syncope and genetic generalized epilepsy in children
Scientific Reports (2023)
-
Diagnostic and societal impact of implementing the syncope guidelines of the European Society of Cardiology (SYNERGY study)
BMC Medicine (2023)
-
Recommendations for tilt table testing and other provocative cardiovascular autonomic tests in conditions that may cause transient loss of consciousness
Clinical Autonomic Research (2021)
-
Classification of orthostatic intolerance through data analytics
Medical & Biological Engineering & Computing (2021)