Key Points
-
Multiple sclerosis (MS) is a chronic immune-mediated demyelinating and neurodegenerative disease, and the main disease-modifying treatments rely on modulation or suppression of the immune system
-
Current results show that most drugs to treat MS are linked to an increased risk of infection to varying degrees, depending on their mode of action
-
Continuous assessment of infectious risks before, during and after disease-modifying therapy for MS, especially when using intravenous drugs, has increasing clinical relevance
-
Experience with the recently approved oral MS disease-modifying therapies illustrates that even after approval, new treatment-associated infectious risks must be taken into account
-
With an increasing number of treatment-associated infections, accurate diagnostic work-up of patients with MS who present with new neurological symptoms becomes crucial
-
Owing to the possibly serious or even fatal complications of modern MS treatment options, safety data on infections must be collected and evaluated in specific databases following drug approval
Abstract
Immunomodulatory and immunosuppressive treatments for multiple sclerosis (MS) are associated with an increased risk of infection, which makes treatment of this condition challenging in daily clinical practice. Use of the expanding range of available drugs to treat MS requires extensive knowledge of treatment-associated infections, risk-minimizing strategies and approaches to monitoring and treatment of such adverse events. An interdisciplinary approach to evaluate the infectious events associated with available MS treatments has become increasingly relevant. In addition, individual stratification of treatment-related infectious risks is necessary when choosing therapies for patients with MS, as well as during and after therapy. Determination of the individual risk of infection following serial administration of different immunotherapies is also crucial. Here, we review the modes of action of the available MS drugs, and relate this information to the current knowledge of drug-specific infectious risks and risk-minimizing strategies.
Similar content being viewed by others
Main
Multiple sclerosis (MS) is an immune-mediated demyelinating and neurodegenerative disease1,2,3,4 that can give rise to heterogeneous clinical presentations5. This condition causes permanent cumulative disability, impairs quality of life and shortens life expectancy. Over the past few years, new disease-modifying therapies for MS have become available, and have prompted changes in treatment algorithms6,7,8. As immunomodulatory treatment options for MS have become more efficient, the associated risk of adverse events, such as infections, has increased9,10,11,12,13.
The different available treatments influence the immune system in distinct ways (Table 1) and, therefore, lead to specific infectious adverse effects14,15,16,17 (Table 2). For some treatment options, specific parameters have been identified that might predict the risk of infection. For example, dimethyl fumarate (DMF) treatment seems to be associated with long-lasting leukopenia and lymphopenia, whereas natalizumab treatment alters leukocyte function, leading to reduced leukocyte infiltration into the CNS and compromised local immune responses. The proper evaluation of the specific infections linked to each MS treatment will, hopefully, contribute to reducing the risk of treatment-associated infections, and to the customization of therapies for individual patients (Table 3).
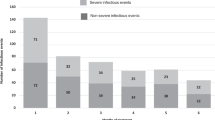
The added risk of infection due to each MS drug is difficult to estimate, as the majority of patients receive treatment, and the correlation between the mode of action and the individual infectious risk of each agent remains unproven in most cases. Some placebo-controlled trials have allowed researchers to identify the 'background' rate of severe infections in patients with MS, which ranges from 0.2% to 2.6%18,19,20,21. Here, we review the mode of action of the current therapies for MS, focusing on the newer disease-modifying treatments (DMTs), and summarize the associated infectious risks along with their clinical implications.
Treatment of relapses
The overall goal of MS management is to control disease activity, halt progression and, ideally, induce reversal of neurological deficits. This endeavour involves long-term administration of disease-modifying drugs.
Two-thirds of patients experience a relapsing–remitting form of the disease. New or reoccurring focal neurological deficits or signs in the context of MS are considered to be relapses22. These relapses are usually treated with pulsed high doses of glucocorticosteroids, and steroid-refractory relapses can be treated with plasmapheresis. The anti-inflammatory effects of these treatment options attenuate acute exacerbations and hasten recovery. In contrast to DMTs, which are aimed at reducing disease activity, as reflected by the annual relapse rate and disease progression, the treatment of relapses is an acute intervention.
Glucocorticosteroids
In general, most patients start with relapsing–remitting MS (RRMS) which, over time, evolves into secondary progressive MS (SPMS). A minority of patients never present with RRMS but experience primary progressive MS (PPMS) from the start. Glucocorticosteroids are mainly used in high doses for short periods of time (0.5–3.0 g daily for 3–5 days, for example) to treat acute exacerbations in MS23,24,25,26. Although convincing class I evidence is lacking, repeated pulse therapy (every 3 months, for example) is also used in occasional patients with SPMS or PPMS23,24,27. Mechanistically, glucocorticosteroids have pleiotropic effects: they curtail the production of numerous inflammatory mediators and attenuate the migration of immune cells across the blood–brain barrier.
Long-term continuous glucocorticosteroid administration, which is not typically used in the treatment of MS, is associated with bacterial, viral, fungal and parasitic infections28. Patients receiving this uninterrupted therapy, to treat rheumatoid arthritis for example, are susceptible to more-severe courses of infection, and the treatment might reactivate dormant conditions29. Moreover, clinical signs of infection can be diminished or masked by glucocorticoid treatment, making localization of the infection site more difficult.
The association between pulsed high-dose glucocorticosteroid treatment and serious infectious complications is less clear. In contrast to continuous treatment, repeated pulse therapy, even at very high doses, does not increase the propensity to develop bacterial or fungal infections, but severe viral infections, such as varicella zoster virus (VZV) or herpes simplex virus (HSV), can develop30 (Table 2). Therefore, it is advisable to routinely test for some of these potentially masked infections during the treatment of MS with glucocorticosteroids31,32 (Table 3).
Plasmapheresis
Plasmapheresis (also known as plasma exchange), which rapidly removes pathogenic substances such as autoantibodies, immune complexes and cytokines from the circulation, can be a therapeutic option in glucocorticosteroid-refractory MS relapses33,34,35,36,37. In general, five to eight courses of plasmapheresis are used as escalating treatment. Plasmapheresis is an invasive therapy that exposes the patient to the risk of infection, primarily through the central venous catheter but also via the elimination of immunoglobulins or complement components38.
Several small studies and case series that involved patients with MS and with other diseases reported different rates of infectious complications associated with plasmapheresis34,39,40,41. In larger studies, the reported incidence of catheter-associated complications ranges from 0.5% to 3.3% in patients with chronic hepatitis C, Guillain–Barré syndrome or other neurological diseases42,43,44. A series of 1,283 plasmapheresis treatments in 79 patients with neurological conditions did not reveal any severe adverse effects or infection with hepatitis B, hepatitis C or HIV42. Similarly, no plasmapheresis-associated infections were detected in 2,502 plasmapheresis sessions in a cohort of 335 patients (among which over 90% had neurological diseases)45 or in a smaller study of 154 courses of plasmapheresis in 17 patients with neurological conditions46. Transmission of viral infections becomes more frequent if plasmapheresis requires the use of fresh frozen plasma rather than albumin34,47,48.
Disease-modifying treatments
DMTs are used to attenuate or silence disease activity through long-term modulation of inflammation and normalization of aberrant immune responses, all of which translates into reduced relapse rates and disease progression, and disability improvement. DMTs can broadly be categorized into recombinant cytokines, complex peptide mixtures, monoclonal antibodies and small molecules.
Injectable agents
IFN-β. For over 20 years, IFN-β has been used to treat RRMS, SPMS and clinically isolated syndrome (CIS). The mechanism of action of IFN-β is complex and involves downregulation of immune recognition molecules such as MHC class II antigens, co-stimulatory molecules and adhesion molecules, modulation of the balance between proinflammatory and anti-inflammatory cytokines, reduction of lymphocyte migration across the blood–brain barrier and, potentially, stimulation of neuronal growth factor release (Table 1). IFN-β1a is administered by weekly intramuscular injection at 30 μg, or by thrice-weekly subcutaneous injections at 22 μg or 44 μg. IFN-β1b is administered by subcutaneous injection at 250 μg every second day.
The phase III studies that led to the licensing of subcutaneous injections of IFN-β1b49 and IFN-β1a50 and intramuscular injections of IFN-β1a51 for the treatment of RRMS did not reveal an increased risk of infectious adverse effects. In addition, 20 years of real-life experience have not uncovered an increased prevalence of specific infections in IFN-β-treated patients, despite treatment-associated leukopenia, with the exception of occasional local infections or abscess formation at the injection site. Like other interferons, the recently licensed pegylated IFN-β1a has not been associated with an increased risk of infection52,53. The first case of progressive multifocal leukoencephalopathy (PML) (Box 1) associated with IFN-β1a monotherapy was reported recently54. However, the patient had an underlying common variable immunodeficiency syndrome with hypogammaglobulinaemia, which probably caused the PML.
Overall, treatment with IFN-β does not carry an increased risk of infection (most notably, opportunistic infections) (Table 2), possibly owing to the involvement of the interferon type I signalling pathway in the defence against viral infections55. Nevertheless, regular monitoring of complete blood counts (CBC) is recommended during treatment.
Glatiramer acetate. Glatiramer acetate is a synthetic polymer that diminishes the expression of MHC class II molecules, deactivates monocytes and macrophages, shifts the cytokine profile from a proinflammatory T-helper 1 (TH1) to an anti-inflammatory TH2 phenotype, and could exert neuroprotective effects (Table 1). The drug is administered by daily subcutaneous injection at a dose of 20 mg to patients with CIS or RRMS56. In light of the results of the GALA study57, the licence for glatiramer acetate was extended to the treatment of mild and moderate RRMS at a dose of 40 mg injected subcutaneously thrice weekly.
During treatment with all doses of glatiramer acetate, individual cases presented with changes in CBC, including leukocytosis or leukopenia, and morphological changes in lymphocytes. HSV infections and vaginal candidiasis were 2% more frequent in patients treated with glatiramer acetate (both treatment regimens) than in placebo-treated patients, whereas other infections, such as abscesses, cellulitis, boils, shingles or pyelonephritis, were rarer with glatiramer acetate treatment than with placebo58. According to the manufacturers' prescribing information, no specific laboratory parameters need to be checked during glatiramer acetate treatment, and no opportunistic infections have been described to be associated with administration of the drug.
Oral drugs
Fingolimod. Fingolimod, a first-in-class sphingosine-1-phosphate (S1P) receptor modulator, was the first oral drug to be approved for the treatment of MS. S1P receptor engagement on T cells blocks their emigration from lymph nodes into the CNS. The action of fingolimod on S1P receptors displayed by glial cells could also promote reparative processes59 (Table 1). Under the terms of the FDA licence, fingolimod can be used as a first-line option to treat RRMS, and the European Medicines Agency (EMA) has approved its use for highly active MS.
The phase III studies that led to marketing approval of fingolimod administration at 0.5 mg daily found similar overall infection rates with and without the drug (TRANSFORMS study: 51% versus 53%; FREEDOMS study: 69% versus 72%) but higher rates of lower respiratory tract infections in fingolimod-treated patients than in the placebo group18,19. Serious infections developed in 1.6% (fingolimod 0.5 mg daily) and 2.6% (fingolimod 1.25 mg daily) of the treated patients compared with 1.9% in patients who received the placebo, with two fatal infections, one case of herpes simplex encephalitis and another of VZV infection in patients treated with 1.25 mg fingolimod18,60,61. An integrated safety analysis of more than 3,500 patients with MS included in licensing trials60 did not reveal an elevated risk of infectious adverse effects, including severe HSV infections, when fingolimod was compared with placebo. These results were in line with the findings of the FREEDOMS trial18. The incidence of VZV infections in patients treated with 0.5 mg fingolimod was 7 per 1,000 patient-years in the postmarketing phase, and 11 per 1,000 patient-years (versus 6 in 1,000 patient-years in the placebo group) in another integrated analysis of phase II and III trials and uncontrolled extension studies62.
Before treatment, the patients participating in the trials were required to be tested for VZV seroprotection — an assessment that is generally recommended before initiation of fingolimod. Seronegative individuals should be vaccinated against varicella if possible63. Nonetheless, even in seroprotected patients, immunity can be impaired during fingolimod treatment and VZV infections or HSV-associated encephalitis can occur64,65.
In addition to VZV and HSV infections, postmarketing surveillance revealed other types of cerebral infections potentially associated with fingolimod treatment (Table 2). Reports of single cases of cryptococcal brain and skin infections66,67,68 have prompted an update of the prescribing information to include the potential risk of cryptococcal infection. In 2015, the manufacturer of fingolimod also reported a case of progressive PML in a patient with no record of previous immunosuppressive treatment, who had been treated with this drug for 4 years. The patient was diagnosed after lesions characteristic of the disease were found on a routine cerebral MRI scan, and traces of the JC virus (JCV), which causes PML69, were detected in the cerebrospinal fluid (CSF). Fingolimod treatment was stopped and the patient did not develop further clinical signs of PML. Other cases of PML have been described in association with fingolimod use, but they were all linked to pretreatment with natalizumab and other immunosuppressive agents70 (Table 2).
A further case of PML was reported in June 2015 in a 54-year-old patient with a 16-year history of MS who had received fingolimod for 2.5 years. He had also been exposed for 4 years to mesalazine (5-aminosalicylic acid) for ulcerative colitis (Novartis, personal communication). During treatment, lymphocytes were within the therapeutic range (0.33–0.55 × 109 cells per l). The patient developed difficulties walking, along with hemiparesis, apathy and stereotyped movements. An MRI scan revealed changes compatible with PML, and JCV DNA was detected in the CSF.
Fingolimod should be used with awareness of the potential risk of PML, and treatment should be permanently discontinued if PML is suspected70. Furthermore, regular monitoring of differential blood counts and lymphocyte levels is recommended by the EMA and the FDA. German guidelines suggest that complete and differential blood counts should be performed at the start of therapy, after 2 and 4 weeks and, subsequently, every 3–6 months during treatment71. In the event of sustained lymphocyte counts below 0.2 × 109 cells per l, treatment should be discontinued until levels rise above 0.6 × 109 cells per l.
To determine the true magnitude of the infectious risk associated with fingolimod, analysis of large data sets from postmarketing studies is required. However, given the 140,000 patient-years of exposure to the treatment to date, the risk seems to be low.
Dimethyl fumarate and fumaric acid esters. DMF (also known as BG12) is another oral treatment option for MS. In 2013, following the phase III studies DEFINE20 and CONFIRM72,73,74, the FDA and the EMA licensed DMF at a twice-daily dose of 240 mg. This drug acts on MS by attenuating the activity of proinflammatory TH1 and TH17 cells, and by scavenging toxic oxygen metabolites (Table 1).
The placebo-controlled DEFINE study revealed that twice-daily and thrice-daily 240 mg doses of DMF were associated with a comparable occurrence of infection to placebo (64% and 68% versus 65%). Most of the infections reported were nasopharyngeal, affected the upper respiratory tract or urinary tract, or were influenza-like infections. Severe infections were detected in 2% of the patients in all groups, but none of these infections were opportunistic. In patients with lymphocyte counts below 0.5 × 109 cells per l, no severe infections were detected. Overall, this study suggests that DMF does not exacerbate the risk of infection in patients with MS.
In the other pivotal study, CONFIRM, DMF at 240 mg twice or thrice daily was compared with glatiramer acetate treatment or placebo administration. Adverse infectious events were observed in 56% of patients in the two DMF study arms, compared with 50% in the two comparator arms. As in the DEFINE study, infections mainly comprised upper respiratory tract infections, urinary tract infections (UTIs), bronchitis and gastroenteritis. In all groups, infections labelled 'severe' were detected in 2% of the patients. In individuals with lymphocyte counts below 0.5 × 109 cells per l, no severe infections were encountered.
In both DEFINE and CONFIRM, lymphocyte counts in patients declined by about 30% during the first year of DMF treatment, mainly due to a reduction in CD8+ lymphocyte numbers75, and were stable thereafter. Absolute lymphocyte counts below 0.5 × 109 cells per l (National Cancer Institute Common Toxicity Criteria grade 3) were seen in about 6% of the patients treated with DMF20,76.
In 2015, the first case of PML in a patient with MS treated with DMF (Tecfidera®) was published77. The patient had been enrolled in the placebo arm of the DEFINE study, and had a 19-year history of MS. She had previously been treated with glatiramer acetate. During the open-label extension study, she received 240 mg of DMF twice a day. After 1 year, she developed lymphopenia (0.29–0.58 × 109 lymphocytes per l). Due to the onset of gait disturbance, dysarthria, and problems coordinating her left arm, the patient was given high doses of glucocorticosteroids and was subjected to plasmapheresis for management of a suspected relapse of MS, in line with current guidelines. The patient failed to respond to treatment. An MRI scan showed cerebral lesions compatible with PML, and her CSF was positive for JCV DNA.
In July 2015, Biogen communicated a second case of PML associated with DMF administration in a patient with PPMS78. The patient had received DMF for 26 months on an off-label basis, leading to recurrent lymphopenia (lymphocyte counts below 0.30 × 109 cells per l). No other PML risk factors including previous immunosuppressive treatments were identified. Later that year, the manufacturer reported a third DMF-associated PML case78. A patient with RRMS received DMF for 1 year, and repeatedly exhibited lymphocyte counts below 0.5 × 109 cells per l. Again, no other risk factors for PML were identified, and the patient had been pretreated only with subcutaneous injections of IFN-β1a. All three of these patients were anti-JCV antibody-positive at the time of PML diagnosis.
Overall, as of November 2015, four cases of PML during DMF (Tecfidera®) treatment have been reported in patients with MS (Biogen, personal communication)77,78,79. Importantly, DMF treatment (including various formulations of fumaric acid esters) for other diseases, such as psoriasis, has also been shown to be associated with PML78,80,81,82,83,84,85, although most patients with psoriasis carried other risk factors for this infection (history of malignancy, systemic lupus erythematosus, sarcoidosis, myelodysplastic syndrome, cytotoxic or efalizumab treatment), creating uncertainty regarding a causative relationship between PML and DMF78,83,86. Other groups have reported cases of human herpes virus 8-associated Kaposi-sarcoma87 or nocardia infection in patients receiving DMF88.
On the basis of case reports, the EMA recently provided updated recommendations to minimize the risk of PML associated with DMF treatment — changes that also apply to other fumarate medicines79. Baseline MRI and white blood cell counts, including lymphocyte counts, should be performed before embarking on DMF therapy. The blood counts should be repeated every 3 months. Should lymphocyte counts drop below 0.5 × 109 cells per l for more than 6 months, the risk–benefit ratio should be reassessed. If therapy is continued in such patients, they should be considered at increased risk for PML, and should be appropriately monitored for signs and symptoms of new neurological dysfunction. Other lymphocyte thresholds apply in patients treated for psoriasis with fumaric acid esters79.
Future research should establish whether monitoring of white blood cell and differential blood counts, using a critical threshold of 0.5 × 109 lymphocytes per l, will generate sufficient protection for patients against PML during DMF treatment. It should be noted that a case of PML was recently reported in a 64-year-old woman with psoriasis who had been treated for about 2 years with topical glucocorticosteroids and Psorinovo® (a compounded delayed-release form of DMF; compounding pharmacy, Mierlo-Hout, Helmond, Netherlands) and did not have a history of prolonged or severe lymphopenia84. Leukocyte and lymphocyte counts were normal at commencement of therapy and during treatment, although lymphocytes had not been monitored for 19 months before the diagnosis of PML by brain biopsy, and the extent of lymphopenia, if any, during that period is unknown89. In the patient's history, no risk factor for the development of PML other than fumaric acid ester treatment was discovered. We can speculate that impaired lymphocyte function or reduction of lymphocyte subgroups (for example, CD8+ lymphocytes), in addition to the absolute lymphocyte count, contributes to PML risk. PML cases have also been described without detectable underlying risk factors90.
Teriflunomide. Teriflunomide — an antimetabolite that inhibits the enzyme dihydroorotate dehydrogenase, which is essential for de novo pyrimidine synthesis by proliferating T cells — preferentially diminishes the activity of recently antigen-activated T lymphocytes (Table 1). The results of the two phase III trials TEMSO91 and TOWER92 led to the approval of teriflunomide as a first-line treatment for RRMS by the FDA in 2012, and by the EMA in 2013 (Refs 74,93).
In the placebo-controlled TEMSO trial, teriflunomide was well tolerated at doses of 7 mg and 14 mg per day, and severe adverse events affected only a minority of the patients. The incidence of infections was similar in all three study arms (placebo 2.2%, teriflunomide 7 mg 1.6%, and teriflunomide 14 mg 2.5%). The incidence of opportunistic infections was not communicated by the investigators. In the group randomly assigned to receive 14 mg of teriflunomide daily, three patients developed severe pyelonephritis, leading to treatment withdrawal in one case.
During the TOWER trial92, moderate and serious infections occurred at a similar frequency — serious infections 3% and UTIs 1% — in the three treatment groups (teriflunomide 7 mg and 14 mg, and placebo). One patient who received active treatment died from Klebsiella-induced sepsis. In addition, two opportunistic infections were identified: a patient in the placebo group contracted hepatitis C and cytomegalovirus infections, and a patient in the teriflunomide 14 mg arm developed intestinal tuberculosis. The latter patient recovered with standard tuberculostatic therapy. In both cases, the investigators considered the infection to be unrelated to the treatment92.
Analysis of long-term data from the initial phase II trial94, which encompassed up to 8.5 years of experience with teriflunomide treatment,95 and the TOPIC trial96, which investigated teriflunomide treatment of CIS, did not reveal an increased risk of infection associated with teriflunomide treatment. Among the severe adverse events associated with teriflunomide, single cases of appendicitis, bronchitis, pneumonia and UTI were reported, but none led to treatment withdrawal. Neither PML nor other opportunistic infections related to the treatment were reported95.
To minimize the infectious risk related to teriflunomide therapy, CBC should be performed every 2 months on initiation of the treatment, and repeated every 3 months after 6 months of treatment. According to the TOWER trial92, treatment should be discontinued if neutrophil counts drop below 1.0 × 109 cells per l. The German guidelines71 recommend suspension of treatment if absolute lymphocyte counts fall below 0.2 × 109 cells per l.
Azathioprine. The prodrug azathioprine is an antimetabolite, and its immunosuppressive effect derives from its analogy with purines: it inhibits DNA synthesis, mostly affecting highly proliferative cells such as T cells (Table 1). In the absence of alternative treatment options, azathioprine was used to treat RRMS for many years before IFN-β became available97,98,99.
Patients receiving azathioprine are at increased risk of bacterial, viral, fungal, protozoal and opportunistic infections, including reactivation of latent infections100. These infections can have serious or even fatal outcomes. Coadministration with allopurinol, a drug used to treat hyperuricaemia, interferes with the degradation of azathioprine and enhances the risk of agranulocytosis (severe leukopenia)101. The risk of azathioprine-related leukopenia is increased 35-fold in patients who carry the Arg139Cys polymorphism in the NUDT15 gene, which is frequently found in Asian populations102.
Frequent testing (complete and differential blood counts) is essential to both determine the individual dosage of azathioprine and to detect potential adverse effects as early as possible.
Intravenous treatment options
Natalizumab. Natalizumab is a humanized monoclonal antibody that recognizes α4 integrins and disrupts their interaction with the adhesion molecule VCAM-1. These events result in reduced migration of leukocytes from the blood to the CNS, and could also lead to deactivation of T cells that have invaded the CNS parenchyma (Table 1).
The trials that led to the approval of natalizumab for the treatment of relapsing MS (AFFIRM and SENTINEL) showed an overall elevation in the incidence of influenza infections, UTIs, upper respiratory tract infections and nasopharyngitis related to the therapy. Single cases of cryptosporidial diarrhoea, fatal herpes encephalitis and cryptococcal meningitis were also reported21,103,104.
During the AFFIRM study21, 3.2% of the patients treated with natalizumab and 2.6% of the patients receiving the placebo showed severe infections. In the natalizumab-treated group, these serious infections included four cases of pneumonia and five cases of UTI or urosepsis; the remaining infections reported as serious had various causes, and included pilonidal cyst infection, cellulitis, febrile infection, gastroenteritis, cryptosporidial diarrhoea, mononucleosis, osteomyelitis, sinusitis, tonsillitis, viral infection, appendicitis, and an infection of unclear cause. During the SENTINEL study103, 2.7% of patients treated with combination therapy (natalizumab plus IFN-β1a) and 2.9% of patients who received IFN-β1a treatment alone displayed severe infections. In this study, no cases of tuberculosis were reported.
As a consequence of the phase III studies21,103, the prescribing information for natalizumab indicates a generalized risk of developing opportunistic infections105, in particular PML106. The SENTINEL study reported two cases of PML (one of which was recognized after the study was completed), which prompted a transient market withdrawal of natalizumab. A third case of PML was subsequently reported in a natalizumab-treated patient with Crohn disease107.
As of September 2015, the overall incidence of natalizumab-associated PML is 4.03 per 1,000 patients (Biogen internal data, September 2015 safety update on natalizumab). In the 142,000 individuals treated with natalizumab up to March 2015, PML was confirmed in 585 patients with MS and in three patients with Crohn disease. 23% of the patients who developed PML died. Robust evidence indicates that the risk of developing PML in people receiving natalizumab treatment rises when JCV antibodies are present, when patients have a history of immunosuppressive pretreatment, and when treatment duration exceeds 2 years108,109,110. Within this stratification, PML risk ranges from 0.1 in 1,000 to 11 in 1,000 patients (manufacturer's data; Biogen internal data, September 2015 safety update on natalizumab, calculation per treatment epoch)111,112; this risk has recently been recalculated independently, and was found to be 23 in 1,000 patients (cumulative risk beyond 24 months of exposure)111.
No direct antiviral treatment is yet available for PML113. When this condition is diagnosed, discontinuation of natalizumab treatment and rapid removal of the antibody from the patient's circulation by plasmapheresis or immunoadsorption is recommended. Development of immune reconstitution inflammatory syndrome (IRIS) with paradoxical worsening of neurological deficits is a frequent complication114, usually requiring intensive care unit treatment and pulsed high-dose glucocorticosteroid therapy. Patients who are assigned to receive natalizumab must be informed of the potential PML risk and the limited treatment options in the event of such a complication.
Pharmacovigilance (CBC every 6 months), clinical awareness raised by the emergence of any new neurological symptoms during natalizumab treatment (cognitive and behavioural changes, retrochiasmatic visual disturbance, hemiparesis, and/or seizures), and frequent clinical and MRI monitoring are essential to minimize the risk of natalizumab-related PML (Box 1). In high-risk patients, MRI scanning every 3 months after 18 months of natalizumab administration is recommended115. If a patient is negative for JCV antibodies, repeated testing every 6 months is advisable.
The CSF JCV antibody index is suggested as a helpful tool to detect natalizumab-associated PML112,115,116,117. In addition, recent studies have shown that serum or plasma JCV antibody levels can contribute to PML risk stratification in antibody-positive patients with no prior immunosuppressant use118.
Recent observations indicate that PML can manifest up to 6 months after discontinuation of natalizumab treatment. These findings include cases where PML was diagnosed after natalizumab treatment was stopped and a new disease-modifying drug was already established119. Researchers found that patients presenting with PML within 6 months after withdrawal of natalizumab frequently had other PML risk factors120. Follow-up MRI should be performed after termination of natalizumab, even in asymptomatic patients121.
Alemtuzumab. Alemtuzumab, an anti-CD52 humanized monoclonal antibody, depletes B and T cells, and leads, via consecutive repopulation, to a long-lasting reconfiguration of the adaptive immune system with a preponderance of regulatory cells122,123,124 (Table 1). On the basis of concordant results in a large active comparator phase II trial and two phase III trials125,126,127, alemtuzumab is recommended for the treatment of highly active MS. Routine alemtuzumab treatment for MS is administered in annual cycles, with five infusions in the first year and three infusions 12 months later.
In the CARE-MS I trial126, infections were reported to be more frequent with alemtuzumab therapy than with IFN-β1a treatment. Most of the infections (98%) were mild to moderate, and none of the reported infections necessitated treatment discontinuation. Upper respiratory tract and herpes infections were predominant, with no life-threatening or fatal outcomes. One patient from a tuberculosis-endemic region developed pulmonary tuberculosis after alemtuzumab therapy and recovered completely with standard treatment128,129.
The CARE-MS II trial127 also reported a greater incidence of infections in patients treated with alemtuzumab than in those receiving IFN-β1a (77% versus 66%). The most frequently reported infections, which were predominantly of mild to moderate severity, were nasopharyngitis (29% versus 24%), UTIs (21% versus 11%), and upper respiratory tract infections (16% versus 12%). Severe infections, which occurred more often with alemtuzumab treatment than with IFN-β1a treatment (4% versus 1%), included mucocutaneous herpes and fungal infections. VZV reactivation (shingles) required inpatient treatment in two cases. No cases of herpes encephalitis were reported.
In both trials, prophylactic acyclovir treatment for the first month of every cycle of alemtuzumab therapy reduced the proportion of herpes simplex infections (CARE-MS I: 1% versus 3%; CARE-MS II: 0.5% versus 2.8% after the first cycle and 0.4% versus 2.1 after the second cycle), compared with alemtuzumab alone.
One CARE-MS I participant, who was from a tuberculosis-endemic region, developed pulmonary tuberculosis after alemtuzumab therapy, and recovered completely with standard tuberculosis treatment128,129. In the CARE-MS II trial, another patient from a tuberculosis-endemic region, who had received one course of high-dose alemtuzumab (24 mg), developed tuberculosis. Another CARE-MS II participant had a positive tuberculin skin test. Both of the CARE-MS II participants responded well to standard tuberculosis treatment.
To date, no cases of PML have been reported after alemtuzumab administration in patients with MS. However, opportunistic infections, such as PML, have been reported following alemtuzumab treatment for haemato-oncological indications, and in transplant patients who had received prior immunosuppressive or cytotoxic treatments, as well as those undergoing immunosuppressive combination or long-term therapy130,131,132.
Two retrospective cohort studies133,134 found no serious infections associated with alemtuzumab treatment in patients with MS. The majority of the infections reported were caused by herpesviruses, and no cases of Listeria-associated infection were detected. However, with more patients being exposed to alemtuzumab following market approval, reports of Listeria-associated infections during or soon after an alemtuzumab treatment cycle have emerged, and some of the patients developed life-threatening Listeria meningitis. Only one case of Listeria infection was recorded during the premarketing study programme125,135,136.
In addition to making their patients aware of Listeria-associated complications, physicians can recommend the pregnancy diet137, which reduces the risk of Listeria infections through avoidance of consumption of raw fish and meat products, as well as unpasteurized milk and sliced mushrooms, before and after alemtuzumab treatment.
In patients receiving alemtuzumab, monthly laboratory tests are performed in the context of a compulsory risk management programme, predominantly because of the risk of autoimmune haemolysis, immune thrombocytopenia, glomerulonephritis and thyroid disorders. The results of these tests should also be evaluated from the perspective of infections. In addition, if fever, skin rashes or headaches develop, patients should promptly see their physician to exclude relevant and possibly treatable infections.
Mitoxantrone. Mitoxantrone is a type II topoisomerase inhibitor that suppresses macrophages, B cells and T cells, with a preferential effect on helper subsets. On the basis of the outcomes of a number of small trials and the MIMS study138, mitoxantrone is currently used for the treatment of active RRMS or SPMS (Table 1). The dosage in the quarterly treatment cycles depends on body surface area, and is usually 12 mg/m2.
During the MIMS trial, 67% of the patients who received the placebo experienced infections, compared with 85% of patients receiving 5 mg/m2 mitoxantrone and 81% of patients receiving 12 mg/m2 mitoxantrone. Few of these infections were serious and required hospitalization (placebo group: a single case of tonsillitis; 5 mg/m2 group: one case of enteritis, one of UTI and one of viral infection; 12 mg/m2 group: single cases of tonsillitis and endometritis and two cases of UTI).
To avoid extensive bone marrow suppression and consecutive cytopenia, the dose of mitoxantrone is normally adjusted following complete and differential blood cell counts, which are carried out weekly up to 3 weeks after treatment, or once up to 7 days before the next mitoxantrone dose139. Contraindications for the use of mitoxantrone include neutropenia (neutrophil counts <1.5 × 109 cells per l), and severe acute and uncontrolled chronic infections.
Long-term postmarketing experience has confirmed the occurrence of frequent UTIs and upper airway infections with mitoxantrone therapy140. Although cases of septicaemia, pneumonia and opportunistic infections have been described following mitoxantrone treatment, this therapy is not associated with a heightened risk of viral infections overall.
Off-label and future treatment options
Rituximab
Rituximab is a chimaeric monoclonal antibody directed against CD20, a protein primarily expressed at the surface of B-precursor cells and B lymphocytes. Administration of rituximab leads to B-cell depletion141, which impairs T-cell activation and release of proinflammatory cytokines. Rituximab is widely used in rheumatology and haematology, in solid organ transplantation, and off-label in various neurological autoimmune diseases including MS.
A phase II study in patients with RRMS142,143 showed that a single course of rituximab led to a prominent decrease in the number of inflammatory brain lesions (shown by MRI) and in the rate of MS relapses over a period of 48 weeks, as compared with placebo. Overall, infections were reported at a similar incidence for the placebo and rituximab groups (71.4% versus 69.6%). The most common infections in the rituximab group were nasopharyngitis, upper respiratory tract infections, UTIs, and sinusitis. Serious infections were observed in 5.7% of the placebo-treated patients and in 2.9% of the rituximab-treated patients. Clinically significant opportunistic infections have not been linked to rituximab treatment. Although rituximab administration has not been shown to increase the risk of infection in patients with RRMS, this drug has yet to be tested in a phase III study in this population.
The phase II/III OLYMPUS trial compared rituximab treatment with placebo in patients with PPMS144. Overall infections occurred at a similar rate in both groups (65.3% with placebo versus 68.2% with rituximab), but serious adverse infections were reported more often in the rituximab group than in the placebo group (4.5% versus <1%). Of note, the majority of serious infections (nine of 13) developed in patients over 55 years of age.
The German Registry of Autoimmune Diseases, which followed up 56 patients who received rituximab treatment for MS or neuromyelitis optica, found no opportunistic infections, and recorded 0.062 infections per patient-year overall145. In settings other than neurological treatment, this therapy can cause serious infection-related complications, which include new manifestations, reactivation or worsening of viral diseases such as hepatitis B146, PML147,148,149,150,151,152, pneumocystis pneumonia, or tuberculosis153. The frequency of PML in patients treated with rituximab for haematological diseases was below 1 in 10,000. Among 312,000 patients treated with rituximab for rheumatoid arthritis, eight contracted PML, and two additional cases of PML have been described in patients with granulomatosis with polyangiitis. Single cases of PML have also been described in association with off-label use in MS and other diseases (Roche, personal communication).
Ocrelizumab
Ocrelizumab is a fully humanized anti-CD20 B-cell-depleting monoclonal antibody that has been tested in rheumatoid arthritis and MS154,155,156. A phase II study in RRMS157 showed no opportunistic infections associated with the use of ocrelizumab, and serious infections were detected at a similar rate (around 2%) in placebo-treated and ocrelizumab-treated patients.
The results of three phase III studies comparing ocrelizumab and interferon treatments for RRMS (OPERA I and II) and PPMS (ORATORIO)154,155,156 have been presented recently158,159. In patients with RRMS, infectious adverse events (including respiratory tract infections and UTIs) occurred in 52.4% of interferon-treated and 58.4% of ocrelizumab-treated patients; for infectious severe adverse events, the corresponding figures were 2.9% and 1.3%, respectively158. In patients with PPMS, infectious adverse events (including gastroenteritis, and respiratory and urinary tract infections) occurred in 67.8% of the interferon-treated and 69.8% of the ocrelizumab-treated group, and infectious severe adverse events were recorded in 5.9% versus 6.2%, respectively. In the ocrelizumab-treated group, two of four deaths were attributed to pneumonia159.
In contrast to MS, the clinical development of ocrelizumab for rheumatoid arthritis was discontinued after phase II160, owing to an unfavourable risk–benefit ratio. Patients recruited in Asia and treated with 1,000 mg ocrelizumab had an increased risk of serious and opportunistic infections, such as mycobacterial infections, hepatitis B reactivation, histoplasmosis, pneumocystis pneumonia, VZV pneumonia or candida infections160.
To date, ocrelizumab has not been approved for treatment of either RRMS or PPMS. A valid judgement of the infectious risks cannot be made at this point because real-life and long-term data are still missing. Serious infections, as encountered in the rheumatoid arthritis trial, have not been observed in MS studies so far.
Ofatumumab
Ofatumumab is another human anti-CD20 B-cell-directed monoclonal antibody currently undergoing clinical development in MS. In a phase II trial examining three different doses of the antibody delivered in two intravenous infusions, no serious infections were recorded in the 36 patients studied per protocol161.
Daclizumab
Daclizumab is a humanized anti-CD25 monoclonal antibody that modulates IL-2 signalling. This leads to the expansion of regulatory natural killer cells, which are thought to eliminate pathogenic T cells that contribute to inflammation in MS. Daclizumab is currently under regulatory consideration for licensing for RRMS treatment. The phase II CHOICE study162 compared different dosages of daclizumab as an add-on therapy to IFN-β treatment. The other phase II trial, SELECT163, compared two different doses of daclizumab with placebo administration. In these studies, the rate of serious infections was slightly increased in the daclizumab-treated groups, as compared with treatment with placebo or IFN-β alone. However, no opportunistic infections were recorded. No specific pattern of organ system involvement was recognized164.
The phase III trial DECIDE165, which compared daclizumab treatment with IFN-β1a administration, reported infectious adverse events in 65% of daclizumab-treated and 57% of IFN-β1a-treated patients, and serious infections in 4% versus 2% of the patients, respectively. Serious infections reported in more than one patient during the study included UTIs, pneumonia, appendicitis, cellulitis and viral infections, but no cases of PML or infectious encephalitis were detected. To fully estimate the risk–benefit ratio of this drug in MS and before suggesting monitoring measures, the approval decisions of the regulatory authorities should be awaited.
Conclusions and recommendations
The repertoire of immunomodulatory agents to treat MS has recently broadened markedly, offering more-efficient and better-suited therapeutic solutions for patients. However, the risk of infection associated with such therapies is gaining increasing importance when planning treatments and monitoring patients.
Current data suggest that the risk of developing infections can increase with the duration of MS treatment. However, the amount of real-life experience accumulated for each MS therapy varies, which precludes a valid comparison of the risks associated with individual treatments. Long-term treatment with interferons or glatiramer acetate seems to carry a low risk of infections.
Experience with natalizumab, DMF and fingolimod indicates that the most profound risk of the newer DMTs relates to PML and other opportunistic infectious diseases. Management decisions to minimize such risk require comprehensive analysis of multiple aspects, including patient history of infectious disorders, risks of exposure to distinct microorganisms (for example, endemic regions for tuberculosis or parasites), presence of concomitant autoimmune diseases or other comorbidities, history of prior exposure to immunomodulatory or immunosuppressive agents, and the immune status of the patient.
In view of previous clinical experience and published evidence, individual risk stratification is required when choosing immunomodulatory drugs, and rigorous pharmacovigilance is essential. Notably, recent experience shows that infectious risks and serious adverse events might not be recognized during pivotal trial programmes, given the short duration of follow-up, enrolment of selected study populations, and low numbers of patients treated. Therefore, special clinical awareness, comprehensive information and multidisciplinary medical care for patients are urgently needed.
Vaccines have an important role in the prevention of treatment-associated infections, and should be encouraged before the initiation of disease-modifying therapy whenever possible166. The CNS represents a partially privileged compartment, as intact blood–brain and CSF–brain barriers prevent ready access of cellular or humoral immune components to the CNS (except at specific sites). Nevertheless, activated T lymphocytes can patrol the CNS and scan for foreign antigens. If these T cells recognize — for example — viral proteins in the context of MHC class I, they can launch an attack on glial cells or neurons infected with such a virus167.
In consideration of the severe and potentially life-threatening conditions caused by the infectious agents associated with the immunomodulatory agents used to treat MS, the use of specific registries and databases to collect and evaluate infectious safety data after drug approval is advisable.
Clearly, development of new drugs for the treatment of MS should aim not only at augmenting efficacy, but also at increasing safety in terms of potential risks of infections. Ideally, therapeutic strategies that reconfigure the immune system to eliminate or silence the aberrant immunity at the root of the disease process while preserving natural defence mechanisms should be promoted. However this approach might not completely prevent infections from developing, as experience with the newer DMTs has taught us. Further research is required to elucidate the aetiopathogenesis of opportunistic infections — in particular, PML — in the context of immunomodulatory therapies.
References
Lassmann, H. Pathology and disease mechanisms in different stages of multiple sclerosis. J. Neurol. Sci. 333, 1–4 (2013).
Lucchinetti, C. F. et al. Inflammatory cortical demyelination in early multiple sclerosis. N. Engl. J. Med. 365, 2188–2197 (2011).
Mahad, D. H., Trapp, B. D. & Lassmann, H. Pathological mechanisms in progressive multiple sclerosis. Lancet Neurol. 14, 183–193 (2015).
Lassmann, H. Spinal cord pathology in multiple sclerosis. Lancet Neurol. 14, 348–349 (2015).
Zettl, U. K., Stuve, O. & Patejdl, R. Immune-mediated CNS diseases: a review on nosological classification and clinical features. Autoimmun. Rev. 11, 167–173 (2012).
Broadley, S. A. et al. Therapeutic approaches to disease modifying therapy for multiple sclerosis in adults: an Australian and New Zealand perspective: part 3 treatment practicalities and recommendations. MS Neurology Group of the Australian and New Zealand Association of Neurologists. J. Clin. Neurosci. 21, 1857–1865 (2014).
Correale, J. et al. Management of relapsing–remitting multiple sclerosis in Latin America: practical recommendations for treatment optimization. J. Neurol. Sci. 339, 196–206 (2014).
Freedman, M. S. et al. Treatment optimization in MS: Canadian MS Working Group updated recommendations. Can. J. Neurol. Sci. 40, 307–323 (2013).
Aktas, O., Kieseier, B. & Hartung, H. P. Neuroprotection, regeneration and immunomodulation: broadening the therapeutic repertoire in multiple sclerosis. Trends Neurosci. 33, 140–152 (2010).
Jeffery, D. R. Recent advances in treating multiple sclerosis: efficacy, risks and place in therapy. Ther. Adv. Chron. Dis. 4, 45–51 (2013).
Killestein, J., Rudick, R. A. & Polman, C. H. Oral treatment for multiple sclerosis. Lancet Neurol. 10, 1026–1034 (2011).
Meuth, S. G., Gobel, K. & Wiendl, H. Immune therapy of multiple sclerosis — future strategies. Curr. Pharm. Des. 18, 4489–4497 (2012).
Mulakayala, N., Rao, P., Iqbal, J., Bandichhor, R. & Oruganti, S. Synthesis of novel therapeutic agents for the treatment of multiple sclerosis: a brief overview. Eur. J. Med. Chem. 60, 170–186 (2013).
Abinun, M. An overview of infectious complications in children on new biologic response-modifying agents. Pediatr. Health 4, 509–517 (2010).
Afif, W. & Loftus Jr, E. V. Safety profile of IBD therapeutics: infectious risks. Gastroenterol. Clin. North Am. 38, 691–709 (2009).
Breda, L., Del Torto, M., De Sanctis, S. & Chiarelli, F. Biologics in children's autoimmune disorders: efficacy and safety. Eur. J. Pediatr. 170, 157–167 (2011).
Berger, J. R. & Houff, S. Opportunistic infections and other risks with newer multiple sclerosis therapies. Ann. Neurol. 65, 367–377 (2009).
Kappos, L. et al. A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis. N. Engl. J. Med. 362, 387–401 (2010).
Cohen, J. A. et al. Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis. N. Engl. J. Med. 362, 402–415 (2010).
Gold, R. et al. Placebo-controlled Phase 3 study of oral BG-12 for relapsing multiple sclerosis. N. Engl. J. Med. 367, 1098–1107 (2012).
Polman, C. H. et al. A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. N. Engl. J. Med. 354, 899–910 (2006).
McDonald, W. I. et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann. Neurol. 50, 121–127 (2001).
Pirko, I. & Rodriguez, M. Pulsed intravenous methylprednisolone therapy in progressive multiple sclerosis: need for a controlled trial. Arch. Neurol. 61, 1148–1149 (2004).
Goodkin, D. E. et al. A Phase II study of i.v. methylprednisolone in secondary-progressive multiple sclerosis. Neurology 51, 239–245 (1998).
Chinen, J. & Shearer, W. T. Secondary immunodeficiencies, including HIV infection. J. Allergy Clin. Immunol. 125, S195–S203 (2010).
Schweingruber, N., Reichardt, S. D., Luhder, F. & Reichardt, H. M. Mechanisms of glucocorticoids in the control of neuroinflammation. J. Neuroendocrinol. 24, 174–182 (2012).
Rommer, P. S. et al. Patients characteristics influencing the longitudinal utilization of steroids in multiple sclerosis — an observational study. Eur. J. Clin. Invest. 45, 587–593 (2015).
Klein, N. C., Go, C. H. & Cunha, B. A. Infections associated with steroid use. Infect. Dis. Clin. North Am. 15, 423–432 (2001).
Dixon, W. G., Suissa, S. & Hudson, M. The association between systemic glucocorticoid therapy and the risk of infection in patients with rheumatoid arthritis: systematic review and meta-analyses. Arthritis Res. Ther. 13, R139 (2011).
Le Page, E. et al. Oral versus intravenous high-dose methylprednisolone for treatment of relapses in patients with multiple sclerosis (COPOUSEP): a randomised, controlled, double-blind, non-inferiority trial. Lancet 386, 974–981 (2015).
Stahn, C., Lowenberg, M., Hommes, D. W. & Buttgereit, F. Molecular mechanisms of glucocorticoid action and selective glucocorticoid receptor agonists. Mol. Cell. Endocrinol. 275, 71–78 (2007).
Spies, C. M., Bijlsma, J. W., Burmester, G. R. & Buttgereit, F. Pharmacology of glucocorticoids in rheumatoid arthritis. Curr. Opin. Pharmacol. 10, 302–307 (2010).
Weinshenker, B. G. et al. A randomized trial of plasma exchange in acute central nervous system inflammatory demyelinating disease. Ann. Neurol. 46, 878–886 (1999).
Keegan, M. et al. Relation between humoral pathological changes in multiple sclerosis and response to therapeutic plasma exchange. Lancet 366, 579–582 (2005).
Multiple Sclerosis Therapy Consensus Group et al. Basic and escalating immunomodulatory treatments in multiple sclerosis: current therapeutic recommendations. J. Neurol. 255, 1449–1463 (2008).
Ehler, J. et al. Therapeutic plasma exchange in glucocorticosteroid-unresponsive patients with Clinically Isolated Syndrome. Ther. Apher. Dial. 18, 489–496 (2014).
Ehler, J. et al. Response to therapeutic plasma exchange as a rescue treatment in clinically isolated syndromes and acute worsening of multiple sclerosis: a retrospective analysis of 90 patients. PLoS ONE 10, e0134583 (2015).
Lehmann, H. C., Hartung, H. P., Hetzel, G. R., Stuve, O. & Kieseier, B. C. Plasma exchange in neuroimmunological disorders: Part 1: Rationale and treatment of inflammatory central nervous system disorders. Arch. Neurol. 63, 930–935 (2006).
Wing, E. J., Bruns, F. J., Fraley, D. S., Segel, D. P. & Adler, S. Infectious complications with plasmapheresis in rapidly progressive glomerulonephritis. JAMA 244, 2423–2426 (1980).
Mokrzycki, M. H. & Kaplan, A. A. Therapeutic plasma exchange: complications and management. Am. J. Kidney Dis. 23, 817–827 (1994).
Haugh, P. J., Levy, C. S., Smith, M. A. & Walshe, D. K. Nosocomial Neisseria meningitidis sepsis as a complication of plasmapheresis. Clin. Infect. Dis. 22, 1116–1117 (1996).
Vucic, S. & Davies, L. Safety of plasmapheresis in the treatment of neurological disease. Aust. N. Z. J. Med. 28, 301–305 (1998).
Kaneko, S. et al. Efficacy and safety of double filtration plasmapheresis in combination with interferon therapy for chronic hepatitis C. Hepatol. Res. 40, 1072–1081 (2010).
Lin, J. H. et al. Prognostic factors and complication rates for double-filtration plasmapheresis in patients with Guillain–Barré syndrome. Transfus. Apher. Sci. 52, 78–83 (2015).
Yeh, J. H., Chen, W. H. & Chiu, H. C. Complications of double-filtration plasmapheresis. Transfusion 44, 1621–1625 (2004).
Rodnitzky, R. L. & Goeken, J. A. Complications of plasma exchange in neurological patients. Arch. Neurol. 39, 350–354 (1982).
Bouget, J., Chevret, S., Chastang, C. & Raphael, J. C. Plasma exchange morbidity in Guillain–Barré syndrome: results from the French prospective, randomized, multicenter study. The French Cooperative Group. Crit. Care Med. 21, 651–658 (1993).
Boucher, C. A., de Gans, J., van Oers, R., Danner, S. & Goudsmit, J. Transmission of HIV and AIDS by plasmapheresis for Guillain–Barré syndrome. Clin. Neurol. Neurosurg. 90, 235–236 (1988).
[No authors listed.] Interferon beta-1b is effective in relapsing–remitting multiple sclerosis. I. Clinical results of a multicenter, randomized, double-blind, placebo-controlled trial. The IFNB Multiple Sclerosis Study Group. Neurology 43, 655–661 (1993).
Ebers, C. G. Randomised double-blind placebo-controlled study of interferon β-1a in relapsing/remitting multiple sclerosis. Lancet 352, 1498–1504 (1998).
Jacobs, L. D. et al. Intramuscular interferon beta-1a for disease progression in relapsing multiple sclerosis. Ann. Neurol. 39, 285–294 (1996).
Calabresi, P. A. et al. Pegylated interferon β-1a for relapsing–remitting multiple sclerosis (ADVANCE): a randomised, Phase 3, double-blind study. Lancet Neurol. 13, 657–665 (2014).
Kieseier, B. C. et al. Peginterferon beta-1a in multiple sclerosis: 2-year results from ADVANCE. Mult. Scler. 21, 1025–1035 (2014).
Lehmann, H. C., Kruger, K., Fink, G. R. & Schroeter, M. Progressive multifocal leukoencephalopathy after interferon beta-1a monotherapy. J. Neurol. 262, 771–773 (2015).
McGlasson, S., Jury, A., Jackson, A. & Hunt, D. Type I interferon dysregulation and neurological disease. Nat. Rev. Neurol. 11, 515–523 (2015).
Johnson, K. P. et al. Copolymer 1 reduces relapse rate and improves disability in relapsing–remitting multiple sclerosis: results of a Phase III multicenter, double-blind placebo-controlled trial. The Copolymer 1 Multiple Sclerosis Study Group. Neurology 45, 1268–1276 (1995).
Khan, O., Rieckmann, P., Boyko, A., Selmaj, K. & Zivadinov, R. Three times weekly glatiramer acetate in relapsing–remitting multiple sclerosis. Ann. Neurol. 73, 705–713 (2013).
US Food and Drug Administration. Full prescribing information for copaxone (glatiramer acetate). FDA.gov[online], (2009).
Aktas, O., Kury, P., Kieseier, B. & Hartung, H. P. Fingolimod is a potential novel therapy for multiple sclerosis. Nat. Rev. Neurol. 6, 373–382 (2010).
Kappos, L. et al. Fingolimod in relapsing multiple sclerosis: an integrated analysis of safety findings. Mult. Scler. Relat. Disord. 3, 494–504 (2014).
Cohen, J. A. et al. Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis. N. Engl. J. Med. 362, 402–415 (2010).
Arvin, A. M. et al. Varicella-zoster virus infections in patients treated with fingolimod: risk assessment and consensus recommendations for management. JAMANeurol. 72, 31–39 (2015).
Winkelmann, A., Loebermann, M., Reisinger, E. C., Hartung, H. P. & Zettl, U. K. Fingolimod treatment for multiple sclerosis patients. What do we do with varicella? Ann. Neurol. 70, 673–674; author reply 674 (2011).
Issa, N. P. & Hentati, A. VZV encephalitis that developed in an immunized patient during fingolimod therapy. Neurology 84, 99–100 (2015).
Pfender, N., Jelcic, I., Linnebank, M., Schwarz, U. & Martin, R. Reactivation of herpesvirus under fingolimod: a case of severe herpes simplex encephalitis. Neurology 84, 2377–2378 (2015).
Huang, D. Disseminated cryptococcosis in a patient with multiple sclerosis treated with fingolimod. Neurology 85, 1001–1003 (2015).
Achtnichts, L., Obreja, O., Conen, A., Fux, C. A. & Nedeltchev, K. Cryptococcal meningoencephalitis in a patient with multiple sclerosis treated with fingolimod. JAMA Neurol. 72, 1203–1205 (2015).
Forrestel, A. K., Modi, B. G., Longworth, S., Wilck, M. B. & Micheletti, R. G. Primary cutaneous cryptococcus in a patient with multiple sclerosis treated with fingolimod. JAMA Neurol. http://dx.doi.org/10.1001/jamaneurol.2015.4259, (2016).
Wollebo, H. S., White, M. K., Gordon, J., Berger, J. R. & Khalili, K. Persistence and pathogenesis of the neurotropic polyomavirus JC. Ann. Neurol. 77, 560–570 (2015).
[No authors listed.] Dear Doctor letter (rote-hand-brief) on Gilenya® (fingolimod): first reported case of progressive multifocal leukoencephalopathy (PML). Federal Institute for Drugs and Medical Devices [online], (in German) (2015).
[No authors listed.] Fingolimod. Kompetenznetz Multiple Sklerose [online], (in German) (2015).
Fox, R. J. et al. Placebo-controlled Phase 3 study of oral BG-12 or glatiramer in multiple sclerosis. N. Engl. J. Med. 367, 1087–1097 (2012).
[No authors listed.] Tecfidera. European Medicines Agency [online], (2013).
US Food and Drug Administration. FDA approves new multiple sclerosis treatment: Tecfidera. FDA.gov[online], (2013).
Khatri, B. O. et al. The effect of dimethyl fumarate (Tecfidera) on lymphocyte counts: a potential contributor to progressive multifocal leukoencephalopathy risk. Mult. Scler. Relat. Disord. 4, 377–379 (2015).
Spencer, C. M., Crabtree-Hartman, E. C., Lehmann-Horn, K., Cree, B. A. & Zamvil, S. S. Reduction of CD8+ T lymphocytes in multiple sclerosis patients treated with dimethyl fumarate. Neurol. Neuroimmunol. Neuroinflamm. 2, e76 (2015).
Rosenkranz, T., Novas, M. & Terborg, C. PML in a patient with lymphocytopenia treated with dimethyl fumarate. N. Engl. J. Med. 372, 1476–1478 (2015).
[No authors listed.] Tecfidera® (dimethyl fumarate): new measures to minimise the risk of PML — enhanced monitoring and stopping rules. Biogen [online], (2015).
[No authors listed.] Updated recommendations to minimise the risk of the rare brain infection PML with Tecfidera. European Medicines Agency [online], (2015).
Ermis, U., Weis, J. & Schulz, J. B. PML in a patient treated with fumaric acid. N. Engl. J. Med. 368, 1657–1658 (2013).
van Oosten, B. W., Killestein, J., Barkhof, F., Polman, C. H. & Wattjes, M. P. PML in a patient treated with dimethyl fumarate from a compounding pharmacy. N. Engl. J. Med. 368, 1658–1659 (2013).
Sweetser, M. T., Dawson, K. T. & Bozic, C. Manufacturer's response to case reports of PML. N. Engl. J. Med. 368, 1659–1661 (2013).
Stoppe, M. et al. Cerebellar manifestation of PML under fumarate and after efalizumab treatment of psoriasis. J. Neurol. 261, 1021–1024 (2014).
Nieuwkamp, D. J. et al. PML in a patient without severe lymphocytopenia receiving dimethyl fumarate. N. Engl. J. Med. 372, 1474–1476 (2015).
Bartsch, T. et al. Progressive neurologic dysfunction in a psoriasis patient treated with dimethyl fumarate. Ann. Neurol. 78, 501–514 (2015).
Dammeier, N., Schubert, V., Hauser, T. K., Bornemann, A. & Bischof, F. Case report of a patient with progressive multifocal leukoencephalopathy under treatment with dimethyl fumarate. BMC Neurol. 15, 108 (2015).
[No authors listed.] Arzneimittelkommission der deutschen Ärzteschaft – “Aus der UAW-Datenbank”: Reversibles Kaposi-Sarkom unter Fumaderm®-assoziierter Lymphozytopenie. Dtsch. Arztebl. Int. 106, 2380 (in German) (2009).
[No authors listed.] Arzneimittelkommission der Deutschen Ärzteschaft: “Aus der UAW-Datenbank” – Nokardiose bei Lymphopenie durch Fumaderm®. Dtsch. Arztebl. Int. 110, 1220–1221 (in German) (2013).
Reich, K., Hartung, H. P. & Lebwohl, M. More on PML in patients treated with dimethyl fumarate. N. Engl. J. Med. 374, 294–295 (2016).
Gheuens, S., Pierone, G., Peeters, P. & Koralnik, I. J. Progressive multifocal leukoencephalopathy in individuals with minimal or occult immunosuppression. J. Neurol. Neurosurg. Psychiatry 81, 247–254 (2010).
O'Connor, P. et al. Randomized trial of oral teriflunomide for relapsing multiple sclerosis. N. Engl. J. Med. 365, 1293–1303 (2011).
Confavreux, C. et al. Oral teriflunomide for patients with relapsing multiple sclerosis (TOWER): a randomised, double-blind, placebo-controlled, Phase 3 trial. Lancet Neurol. 13, 247–256 (2014).
[No authors listed.] Aubagio. European Medicines Agency [online], (2013).
O'Connor, P. W. et al. A Phase II study of the safety and efficacy of teriflunomide in multiple sclerosis with relapses. Neurology 66, 894–900 (2006).
Confavreux, C. et al. Long-term follow-up of a Phase 2 study of oral teriflunomide in relapsing multiple sclerosis: safety and efficacy results up to 8.5 years. Mult. Scler. 18, 1278–1289 (2012).
Miller, A. E. et al. Oral teriflunomide for patients with a first clinical episode suggestive of multiple sclerosis (TOPIC): a randomised, double-blind, placebo-controlled, Phase 3 trial. Lancet Neurol. 13, 977–986 (2014).
Filippini, G. et al. Immunomodulators and immunosuppressants for multiple sclerosis: a network meta-analysis. Cochrane Database Syst. Rev. 6, CD008933 (2013).
Casetta, I., Iuliano, G. & Filippini, G. Azathioprine for multiple sclerosis. Cochrane Database Syst. Rev. 4, CD003982 (2007).
Yudkin, P. L. et al. Overview of azathioprine treatment in multiple sclerosis. Lancet 338, 1051–1055 (1991).
US Food and Drug Administration. IMURAN (azathioprine). FDA.gov[online], (2014).
Min, M. X., Weinberg, D. I. & McCabe, R. P. Allopurinol enhanced thiopurine treatment for inflammatory bowel disease: safety considerations and guidelines for use. J. Clin. Pharm. Ther. 39, 107–111 (2014).
Yang, S. K. et al. A common missense variant in NUDT15 confers susceptibility to thiopurine-induced leukopenia. Nat. Genet. 46, 1017–1020 (2014).
Rudick, R. A. et al. Natalizumab plus interferon beta-1a for relapsing multiple sclerosis. N. Engl. J. Med. 354, 911–923 (2006).
Valenzuela, R. M., Pula, J. H., Garwacki, D., Cotter, J. & Kattah, J. C. Cryptococcal meningitis in a multiple sclerosis patient taking natalizumab. J. Neurol. Sci. 340, 109–111 (2014).
US Food and Drug Administration. TYSABRI (natalizumab) injection for intravenous use. FDA.gov[online], (2008).
Warnke, C., Olsson, T. & Hartung, H. P. PML: the dark side of immunotherapy in multiple sclerosis. Trends Pharmacol. Sci. 36, 799–801 (2015).
Van Assche, G. et al. Progressive multifocal leukoencephalopathy after natalizumab therapy for Crohn's disease. N. Engl. J. Med. 353, 362–368 (2005).
Sorensen, P. S. et al. Risk stratification for progressive multifocal leukoencephalopathy in patients treated with natalizumab. Mult. Scler. 18, 143–152 (2012).
Bloomgren, G. et al. Risk of natalizumab-associated progressive multifocal leukoencephalopathy. N. Engl. J. Med. 366, 1870–1880 (2012).
Monaco, M. C. & Major, E. O. Immune system involvement in the pathogenesis of JC virus induced PML: what is learned from studies of patients with underlying diseases and therapies as risk factors. Front. Immunol. 6, 159 (2015).
Berger, J. R. & Fox, R. J. Reassessing the risk of natalizumab-associated PML. J. Neurovirol. http://dx.doi.org/10.1007/s13365-016-0427-6, (2016).
McGuigan, C. et al. Stratification and monitoring of natalizumab-associated progressive multifocal leukoencephalopathy risk: recommendations from an expert group. J. Neurol. Neurosurg. Psychiatry 87, 117–125 (2016).
Warnke, C. et al. Natalizumab and progressive multifocal leukoencephalopathy: what are the causal factors and can it be avoided? Arch. Neurol. 67, 923–930 (2010).
Clifford, D. B. et al. Natalizumab-associated progressive multifocal leukoencephalopathy in patients with multiple sclerosis: lessons from 28 cases. Lancet Neurol. 9, 438–446 (2010).
[No authors listed.] Updated recommendations to minimise the risk of the rare brain infection PML with Tysabri. European Medicines Agency [online], (2016).
Warnke, C. et al. Cerebrospinal fluid JC virus antibody index for diagnosis of natalizumab-associated progressive multifocal leukoencephalopathy. Ann. Neurol. 76, 792–801 (2014).
Wattjes, M. P. & Warnke, C. Guidelines on PML risk stratification and diagnosis in patients with MS treated with natalizumab: so far so good? J. Neurol. Neurosurg. Psychiatry 87, 115 (2015).
Plavina, T. et al. Anti-JC virus antibody levels in serum or plasma further define risk of natalizumab-associated progressive multifocal leukoencephalopathy. Ann. Neurol. 76, 802–812 (2014).
Gheuens, S. et al. Progressive multifocal leukoencephalopathy not observed later than 6 months after natalizumab discontinuation (Poster). Presented at the 67th American Academy of Neurology Annual Meeting (2015).
Fine, A. J., Sorbello, A., Kortepeter, C. & Scarazzini, L. Progressive multifocal leukoencephalopathy after natalizumab discontinuation. Ann. Neurol. 75, 108–115 (2014).
Wattjes, M. P. & Killestein, J. Progressive multifocal leukoencephalopathy after natalizumab discontinuation: few and true? Ann. Neurol. 75, 462 (2014).
Cox, A. L. et al. Lymphocyte homeostasis following therapeutic lymphocyte depletion in multiple sclerosis. Eur. J. Immunol. 35, 3332–3342 (2005).
Jones, J. L. et al. IL-21 drives secondary autoimmunity in patients with multiple sclerosis, following therapeutic lymphocyte depletion with alemtuzumab (Campath-1H). J. Clin. Invest. 119, 2052–2061 (2009).
Thompson, S. A., Jones, J. L., Cox, A. L., Compston, D. A. & Coles, A. J. B-cell reconstitution and BAFF after alemtuzumab (Campath-1H) treatment of multiple sclerosis. J. Clin. Immunol. 30, 99–105 (2010).
The CAMMS223 Trial Investigators. Alemtuzumab versus interferon beta-1a in early multiple sclerosis. N. Engl. J. Med. 359, 1786–1801 (2008).
Cohen, J. A. et al. Alemtuzumab versus interferon beta 1a as first-line treatment for patients with relapsing–remitting multiple sclerosis: a randomised controlled Phase 3 trial. Lancet 380, 1819–1828 (2012).
Coles, A. J. et al. Alemtuzumab for patients with relapsing multiple sclerosis after disease-modifying therapy: a randomised controlled Phase 3 trial. Lancet 380, 1829–1839 (2012).
Menge, T., Stuve, O., Kieseier, B. C. & Hartung, H. P. Alemtuzumab: the advantages and challenges of a novel therapy in MS. Neurology 83, 87–97 (2014).
Hartung, H. P., Aktas, O. & Boyko, A. N. Alemtuzumab: a new therapy for active relapsing–remitting multiple sclerosis. Mult. Scler. 21, 22–34 (2015).
Havrdova, E., Horakova, D. & Kovarova, I. Alemtuzumab in the treatment of multiple sclerosis: key clinical trial results and considerations for use. Ther. Adv. Neurol. Disord. 8, 31–45 (2015).
Waggoner, J., Martinu, T. & Palmer, S. M. Progressive multifocal leukoencephalopathy following heightened immunosuppression after lung transplant. J. Heart Lung Transplant. 28, 395–398 (2009).
Isidoro, L., Pires, P., Rito, L. & Cordeiro, G. Progressive multifocal leukoencephalopathy in a patient with chronic lymphocytic leukaemia treated with alemtuzumab. BMJ Case Rep. http://dx.doi.org/10.1136/bcr-2013-201781, (2014).
Tuohy, O. et al. Alemtuzumab treatment of multiple sclerosis: long-term safety and efficacy. J. Neurol. Neurosurg. Psychiatry 86, 208–215 (2015).
Willis, M. D. et al. Alemtuzumab for multiple sclerosis: long term follow-up in a multi-centre cohort. Mult. Scler. http://dx.doi.org/10.1177/1352458515614092, (2015).
Wray, S. A descriptive analysis of infectious adverse events in alemtuzumab treated multiple sclerosis patients. Presented at the 25th Congress of the European Committee for the Treatment and Research In Multiple Sclerosis (2009).
Rau, D. et al. Listeria meningitis complicating alemtuzumab treatment in multiple sclerosis — report of two cases. Int. J. Mol. Sci. 16, 14669–14676 (2015).
Committee on Infectious Diseases & Committee on Nutrition & American Academy of Pediatrics. Consumption of raw or unpasteurized milk and milk products by pregnant women and children. Pediatrics 133, 175–179 (2014).
Hartung, H. P. et al. Mitoxantrone in progressive multiple sclerosis: a placebo-controlled, double-blind, randomised, multicentre trial. Lancet 360, 2018–2025 (2002).
US Food and Drug Administration. NOVANTRONE. FDA.gov[online], (2008).
Martinelli Boneschi, F., Vacchi, L., Rovaris, M., Capra, R. & Comi, G. Mitoxantrone for multiple sclerosis. Cochrane Database Syst. Rev. 5, CD002127 (2013).
Lutterotti, A. & Martin, R. Getting specific: monoclonal antibodies in multiple sclerosis. Lancet Neurol. 7, 538–547 (2008).
Hauser, S. L. et al. B-cell depletion with rituximab in relapsing–remitting multiple sclerosis. N. Engl. J. Med. 358, 676–688 (2008).
He, D. et al. Rituximab for relapsing–remitting multiple sclerosis. Cochrane Database Syst. Rev. 12, CD009130 (2013).
Hawker, K. et al. Rituximab in patients with primary progressive multiple sclerosis: results of a randomized double-blind placebo-controlled multicenter trial. Ann. Neurol. 66, 460–471 (2009).
Rommer, P. S. et al. Safety and clinical outcomes of rituximab treatment in patients with multiple sclerosis and neuromyelitis optica: experience from a national online registry (GRAID). J. Neuroimmune Pharmacol. 11, 1–8 (2016).
Martin, S. T., Cardwell, S. M., Nailor, M. D. & Gabardi, S. Hepatitis B reactivation and rituximab: a new boxed warning and considerations for solid organ transplantation. Am. J. Transplant. 14, 788–796 (2014).
Lanini, S. et al. Risk of infection in patients with lymphoma receiving rituximab: systematic review and meta-analysis. BMC Med. 9, 36 (2011).
Carbone, J., del Pozo, N., Gallego, A. & Sarmiento, E. Immunological risk factors for infection after immunosuppressive and biologic therapies. Expert Rev. Anti Infect. Ther. 9, 405–413 (2011).
Dang, L., Dang, X., Koralnik, I. J. & Todd, P. K. JC polyomavirus granule cell neuronopathy in a patient treated with rituximab. JAMA Neurol. 71, 487–489 (2014).
Carson, K. R. et al. Progressive multifocal leukoencephalopathy after rituximab therapy in HIV-negative patients: a report of 57 cases from the Research on Adverse Drug Events and Reports project. Blood 113, 4834–4840 (2009).
Tony, H. P. et al. Safety and clinical outcomes of rituximab therapy in patients with different autoimmune diseases: experience from a national registry (GRAID). Arthritis Res. Ther. 13, R75 (2011).
Molloy, E. S. & Calabrese, L. H. Progressive multifocal leukoencephalopathy associated with immunosuppressive therapy in rheumatic diseases: evolving role of biologic therapies. Arthritis Rheum. 64, 3043–3051 (2012).
van Vollenhoven, R. F. et al. Long-term safety of rituximab in rheumatoid arthritis: 9.5-year follow-up of the global clinical trial programme with a focus on adverse events of interest in RA patients. Ann. Rheum. Dis. 72, 1496–1502 (2013).
US National Library of Science. ClinicalTrials.gov [online], (2016).
US National Library of Science. ClinicalTrials.gov [online], (2016).
US National Library of Science. ClinicalTrials.gov [online], (2016).
Kappos, L. et al. Ocrelizumab in relapsing–remitting multiple sclerosis: a Phase 2, randomised, placebo-controlled, multicentre trial. Lancet 378, 1779–1787 (2011).
Hauser, S. et al. Efficacy and safety of ocrelizumab in relapsing multiple sklerosis — results of the Phase III double-blind, interferon beta-1a controlled OPERA I and II studies. ECTRIMS Online Library [online], (2015).
Montalban, X. et al. Efficacy and safety of ocrelizumab in primary progressive multiple sclerosis — results of the Phase III, double-blind, placebo controlled ORATORIO study. ECTRIMS Online Library [online], (2015).
Emery, P. et al. Safety with ocrelizumab in rheumatoid arthritis: results from the ocrelizumab Phase III program. PLoS ONE 9, e87379 (2014).
Sorensen, P. S. et al. Safety and efficacy of ofatumumab in relapsing–remitting multiple sclerosis: a Phase 2 study. Neurology 82, 573–581 (2014).
Wynn, D. et al. Daclizumab in active relapsing multiple sclerosis (CHOICE study): a Phase 2, randomised, double-blind, placebo-controlled, add-on trial with interferon beta. Lancet Neurol. 9, 381–390 (2010).
Gold, R. et al. Daclizumab high-yield process in relapsing–remitting multiple sclerosis (SELECT): a randomised, double-blind, placebo-controlled trial. Lancet 381, 2167–2175 (2013).
Pfender, N. & Martin, R. Daclizumab (anti-CD25) in multiple sclerosis. Exp. Neurol. 262 Pt A, 44–51 (2014).
Kappos, L. et al. Daclizumab HYP versus interferon beta-1a in relapsing multiple sclerosis. N. Engl. J. Med. 373, 1418–1428 (2015).
Loebermann, M. et al. Vaccination against infection in patients with multiple sclerosis. Nat. Rev. Neurol. 8, 143–151 (2011).
Russo, M. V. & McGavern, D. B. Immune surveillance of the CNS following infection and injury. Trends Immunol. 36, 637–650 (2015).
Dong-Si, T. et al. Outcome and survival of asymptomatic PML in natalizumab-treated MS patients. Ann. Clin. Transl. Neurol. 1, 755–764 (2014).
Dong-Si, T. et al. Predictors of survival and functional outcomes in natalizumab-associated progressive multifocal leukoencephalopathy. J. Neurovirol. 21, 637–644 (2015).
Baldwin, K. J. & Hogg, J. P. Progressive multifocal leukoencephalopathy in patients with multiple sclerosis. Curr. Opin. Neurol. 26, 318–323 (2013).
Wattjes, M. P. & Barkhof, F. Diagnosis of natalizumab-associated progressive multifocal leukoencephalopathy using MRI. Curr. Opin. Neurol. 27, 260–270 (2014).
Wattjes, M. P. et al. Diagnostic performance of brain MRI in pharmacovigilance of natalizumab-treated MS patients. Mult. Scler. http://dx.doi.org/10.1177/1352458515615225, (2015).
Chahin, S. & Berger, J. R. A risk classification for immunosuppressive treatment-associated progressive multifocal leukoencephalopathy. J. Neurovirol. 21, 623–631 (2015).
Clifford, D. B. Neurological immune reconstitution inflammatory response: riding the tide of immune recovery. Curr. Opin. Neurol. 28, 295–301 (2015).
Brickelmaier, M. et al. Identification and characterization of mefloquine efficacy against JC virus in vitro. Antimicrob. Agents Chemother. 53, 1840–1849 (2009).
Elphick, G. F. et al. The human polyomavirus, JCV, uses serotonin receptors to infect cells. Science 306, 1380–1383 (2004).
Cettomai, D. & McArthur, J. C. Mirtazapine use in human immunodeficiency virus-infected patients with progressive multifocal leukoencephalopathy. Arch. Neurol. 66, 255–258 (2009).
Schroder, A. et al. Successful management of natalizumab-associated progressive multifocal leukoencephalopathy and immune reconstitution syndrome in a patient with multiple sclerosis. Arch. Neurol. 67, 1391–1394 (2010).
Alstadhaug, K. B. et al. Treatment of progressive multifocal leukoencephalopathy with interleukin 7. JAMA Neurol. 71, 1030–1035 (2014).
Berger, B. et al. Severe disease reactivation in four patients with relapsing–remitting multiple sclerosis after fingolimod cessation. J. Neuroimmunol. 282, 118–122 (2015).
Buttgereit, F., Burmester, G. R., Straub, R. H., Seibel, M. J. & Zhou, H. Exogenous and endogenous glucocorticoids in rheumatic diseases. Arthritis Rheum. 63, 1–9 (2011).
Buttgereit, F. A fresh look at glucocorticoids. How to use an old ally more effectively. Bull. NYU Hosp. Jt Dis. 70 (Suppl. 1), 26–29 (2012).
Lehmann, H. C. & Hartung, H. P. Plasma exchange and intravenous immunoglobulins: mechanism of action in immune-mediated neuropathies. J. Neuroimmunol. 231, 61–69 (2011).
Hu, X. et al. A novel PEGylated interferon beta-1a for multiple sclerosis: safety, pharmacology, and biology. J. Clin. Pharmacol. 52, 798–808 (2012).
Caliceti, P. & Veronese, F. M. Pharmacokinetic and biodistribution properties of poly(ethylene glycol)-protein conjugates. Adv. Drug Deliv. Rev. 55, 1261–1277 (2003).
Fensterl, V. & Sen, G. C. Interferons and viral infections. Biofactors 35, 14–20 (2009).
Hundeshagen, A. et al. Elevated type I interferon-like activity in a subset of multiple sclerosis patients: molecular basis and clinical relevance. J. Neuroinflamm. 9, 140 (2012).
Hecker, M. et al. Network analysis of transcriptional regulation in response to intramuscular interferon-beta-1a multiple sclerosis treatment. Pharmacogenom. J. 12, 360 (2012).
Bongioanni, P., Lombardo, F., Moscato, G., Mosti, S. & Meucci, G. T-cell interferon gamma receptor binding in interferon beta-1b-treated patients with multiple sclerosis. Arch. Neurol. 56, 217–222 (1999).
Noronha, A., Toscas, A. & Jensen, M. A. Interferon beta augments suppressor cell function in multiple sclerosis. Ann. Neurol. 27, 207–210 (1990).
Arnason, B. G. Interferon beta in multiple sclerosis. Clin. Immunol. Immunopathol. 81, 1–11 (1996).
Arnason, B. G. et al. Mechanisms of action of interferon-β in multiple sclerosis. Springer Semin. Immunopathol. 18, 125–148 (1996).
Ozenci, V., Kouwenhoven, M., Huang, Y. M., Kivisakk, P. & Link, H. Multiple sclerosis is associated with an imbalance between tumour necrosis factor-alpha (TNF-α)- and IL-10-secreting blood cells that is corrected by interferon-beta (IFN-β) treatment. Clin. Exp. Immunol. 120, 147–153 (2000).
Shapiro, S., Galboiz, Y., Lahat, N., Kinarty, A. & Miller, A. The 'immunological-synapse' at its APC side in relapsing and secondary-progressive multiple sclerosis: modulation by interferon-β. J. Neuroimmunol. 144, 116–124 (2003).
Yushchenko, M. et al. Interferon-β-1 b decreased matrix metalloproteinase-9 serum levels in primary progressive multiple sclerosis. J. Neurol. 250, 1224–1228 (2003).
Boster, A., Bartoszek, M. P., O'Connell, C., Pitt, D. & Racke, M. Efficacy, safety, and cost-effectiveness of glatiramer acetate in the treatment of relapsing–remitting multiple sclerosis. Ther. Adv. Neurol. Disord. 4, 319–332 (2011).
Ziemssen, T., Kumpfel, T., Klinkert, W. E., Neuhaus, O. & Hohlfeld, R. Glatiramer acetate-specific T-helper 1- and 2-type cell lines produce BDNF: implications for multiple sclerosis therapy. Brain 125, 2381–2391 (2002).
Hong, J., Li, N., Zhang, X., Zheng, B. & Zhang, J. Z. Induction of CD4+CD25+ regulatory T cells by copolymer-I through activation of transcription factor Foxp3. Proc. Natl Acad. Sci. USA 102, 6449–6454 (2005).
Teitelbaum, D., Milo, R., Arnon, R. & Sela, M. Synthetic copolymer 1 inhibits human T-cell lines specific for myelin basic protein. Proc. Natl Acad. Sci. USA 89, 137–141 (1992).
Fridkis-Hareli, M. & Strominger, J. L. Promiscuous binding of synthetic copolymer 1 to purified HLA-DR molecules. J. Immunol. 160, 4386–4397 (1998).
O'Sullivan, C. & Dev, K. K. The structure and function of the S1P1 receptor. Trends Pharmacol. Sci. 34, 401–412 (2013).
Cohen, J. A. & Chun, J. Mechanisms of fingolimod's efficacy and adverse effects in multiple sclerosis. Ann. Neurol. 69, 759–777 (2011).
Chanvillard, C., Jacolik, R. F., Infante-Duarte, C. & Nayak, R. C. The role of natural killer cells in multiple sclerosis and their therapeutic implications. Front. Immunol. 4, 63 (2013).
Matloubian, M. et al. Lymphocyte egress from thymus and peripheral lymphoid organs is dependent on S1P receptor 1. Nature 427, 355–360 (2004).
Mandala, S. et al. Alteration of lymphocyte trafficking by sphingosine-1-phosphate receptor agonists. Science 296, 346–349 (2002).
Coelho, R. P., Payne, S. G., Bittman, R., Spiegel, S. & Sato-Bigbee, C. The immunomodulator FTY720 has a direct cytoprotective effect in oligodendrocyte progenitors. J. Pharmacol. Exp. Ther. 323, 626–635 (2007).
Miron, V. E. et al. Fingolimod (FTY720) enhances remyelination following demyelination of organotypic cerebellar slices. Am. J. Pathol. 176, 2682–2694 (2010).
Kohne, A. et al. Fingolimod impedes Schwann cell-mediated myelination: implications for the treatment of immune neuropathies? Arch. Neurol. 69, 1280–1289 (2012).
Mullershausen, F. et al. Phosphorylated FTY720 promotes astrocyte migration through sphingosine-1-phosphate receptors. J. Neurochem. 102, 1151–1161 (2007).
Xie, J. H. et al. Sphingosine-1-phosphate receptor agonism impairs the efficiency of the local immune response by altering trafficking of naive and antigen-activated CD4+ T cells. J. Immunol. 170, 3662–3670 (2003).
Gold, R., Linker, R. A. & Stangel, M. Fumaric acid and its esters: an emerging treatment for multiple sclerosis with antioxidative mechanism of action. Clin. Immunol. 142, 44–48 (2012).
Linker, R. A. et al. Fumaric acid esters exert neuroprotective effects in neuroinflammation via activation of the Nrf2 antioxidant pathway. Brain 134, 678–692 (2011).
Scannevin, R. H. et al. Fumarates promote cytoprotection of central nervous system cells against oxidative stress via the nuclear factor (erythroid-derived 2)-like 2 pathway. J. Pharmacol. Exp. Ther. 341, 274–284 (2012).
Fox, R. I. et al. Mechanism of action for leflunomide in rheumatoid arthritis. Clin. Immunol. 93, 198–208 (1999).
Bar-Or, A., Pachner, A., Menguy-Vacheron, F., Kaplan, J. & Wiendl, H. Teriflunomide and its mechanism of action in multiple sclerosis. Drugs 74, 659–674 (2014).
Elion, G. B. The George Hitchings and Gertrude Elion lecture. Ann. N. Y. Acad. Sci. 685, 400–407 (1993).
Rice, G. P., Hartung, H. P. & Calabresi, P. A. Anti-α4 integrin therapy for multiple sclerosis: mechanisms and rationale. Neurology 64, 1336–1342 (2005).
Leussink, V. I. et al. Blockade of signaling via the very late antigen (VLA-4) and its counterligand vascular cell adhesion molecule-1 (VCAM-1) causes increased T cell apoptosis in experimental autoimmune neuritis. Acta Neuropathol. 103, 131–136 (2002).
Wiendl, H. & Kieseier, B. Multiple sclerosis: reprogramming the immune repertoire with alemtuzumab in MS. Nat. Rev. Neurol. 9, 125–126 (2013).
Xia, M. Q. et al. Structure of the CAMPATH-1 antigen, a glycosylphosphatidylinositol-anchored glycoprotein which is an exceptionally good target for complement lysis. Biochem. J. 293, 633–640 (1993).
Koeller, J. & Eble, M. Mitoxantrone: a novel anthracycline derivative. Clin. Pharm. 7, 574–581 (1988).
Marriott, J. J. et al. Evidence report: the efficacy and safety of mitoxantrone (Novantrone) in the treatment of multiple sclerosis: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 74, 1463–1470 (2010).
Burns, S. A. et al. Mitoxantrone repression of astrocyte activation: relevance to multiple sclerosis. Brain Res. 1473, 236–241 (2012).
Fidler, J. M., DeJoy, S. Q. & Gibbons, J. J. Jr. Selective immunomodulation by the antineoplastic agent mitoxantrone. I. Suppression of B lymphocyte function. J. Immunol. 137, 727–732 (1986).
Riminton, D. S., Hartung, H. P. & Reddel, S. W. Managing the risks of immunosuppression. Curr. Opin. Neurol. 24, 217–223 (2011).
Winkelmann, A., Löbermann, M., Reisinger, E. C. & Zettl, U. K. Infektionen und Infektionsprävention bei Multipler Sklerose. Fragen und Antworten für die klinische Praxis. Nervenheilkunde 33, 883–890 (in German) (2014).
Winkelmann, A., Löbermann, M., Reisinger, E. C. & Zettl, U. K. Multiple sclerosis and infections. Akt. Neurol. 38, 339–350 (in German) (2011).
Frau, J. et al. Role of interferon-beta in Mycobacterium avium subspecies paratuberculosis antibody response in Sardinian MS patients. J. Neurol. Sci. 349, 249–250 (2015).
Chan, H. L., Ren, H., Chow, W. C., Wee, T. & Interferon Beta-1a Hepatitis C Study Group. Randomized trial of interferon beta-1a with or without ribavirin in Asian patients with chronic hepatitis C. Hepatology 46, 315–323 (2007).
Eisenberg, M. et al. Preliminary trial of recombinant fibroblast interferon in chronic hepatitis B virus infection. Antimicrob. Agents Chemother. 29, 122–126 (1986).
Mader, E. C. Jr et al. Tumefactive multiple sclerosis and hepatitis C virus 2a/2C infection: dual benefit of long-term interferon beta-1a therapy? J. Neurol. Sci. 349, 239–242 (2015).
Rao, H. Y. et al. Liver fibrosis and hepatic stellate cells improvement of chronic hepatitis C patients by interferon-β-1a with or without sustained viral response. Hepatogastroenterology 56, 328–334 (2009).
Tan, F. U., Cetinkaya, H., Erden, E., Ulkatan, S. & Aydin, N. Dual benefit from intramuscular interferon-β treatment in a patient with multiple sclerosis and chronic hepatitis-C virus infection. Hepatogastroenterology 49, 1686–1687 (2002).
Khouri, R. et al. IFN-β impairs superoxide-dependent parasite killing in human macrophages: evidence for a deleterious role of SOD1 in cutaneous leishmaniasis. J. Immunol. 182, 2525–2531 (2009).
Maffione, A. B. et al. In vivo effects of recombinant-interferon-β1b treatment on polymorphonuclear cell and monocyte functions and on T-cell-mediated antibacterial activity in patients with relapsing–remitting multiple sclerosis. Immunopharmacol. Immunotoxicol. 22, 1–18 (2000).
Mattner, J. et al. Protection against progressive leishmaniasis by IFN-β. J. Immunol. 172, 7574–7582 (2004).
Olberg, H. K. et al. Immunotherapies influence the influenza vaccination response in multiple sclerosis patients: an explorative study. Mult. Scler. 20, 1074–1080 (2014).
Smith, M. Y. et al. Postmarketing safety profile of subcutaneous interferon beta-1a given 3 times weekly: a retrospective administrative claims analysis. J. Manag. Care Spec. Pharm. 21, 650–660 (2015).
US Food and Drug Administration. FDA drug, safety communication: FDA warns about cases of rare brain infection with MS drug Gilenya (fingolimod) in two patients with no prior exposure to immunosuppressant drugs. FDA.gov[online], (2015).
Ermis, U., Weis, J. & Schulz, J. B. Case reports of PML in patients treated for psoriasis. N. Engl. J. Med. 369, 1081 (2013).
Comi, G. et al. Pooled safety and tolerability data from four placebo-controlled teriflunomide studies and extensions. Mult. Scler. Relat. Disord. 5, 97–104 (2016).
Casetta, I., Iuliano, G. & Filippini, G. Azathioprine for multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 80, 131–132; discussion 132 (2009).
Dahdaleh, D., Altmann, D. M., Malik, O. & Nicholas, R. S. Breathlessness, night sweats, and weight loss on natalizumab. Lancet 380, 726–727 (2012).
de Masson, A. et al. Cavitary pulmonary disease in a patient treated with natalizumab. Presse Med. 43, 1009–1012 (2014).
Hradilek, P., Zeman, D., Tudik, I., Zapletalova, O. & Ulmann, V. Asymptomatic lung disease caused by Mycobacterium kansasii as an opportunistic infection in a patient treated with natalizumab for relapsing–remitting multiple sclerosis. Mult. Scler. 20, 639–640 (2014).
Kohlmann, R. et al. Serological evidence of increased susceptibility to varicella-zoster virus reactivation or reinfection in natalizumab-treated patients with multiple sclerosis. Mult. Scler. 21, 1823–1832 (2015).
Kobeleva, X. et al. Varicella zoster-associated retinal and central nervous system vasculitis in a patient with multiple sclerosis treated with natalizumab. J. Neuroinflamm. 11, 19 (2014).
Kwiatkowski, A. et al. Herpes encephalitis during natalizumab treatment in multiple sclerosis. Mult. Scler. 18, 909–911 (2012).
Sharma, K., Ballham, S. A., Inglis, K. E., Renowden, S. & Cottrell, D. A. Does natalizumab treatment increase the risk of herpes simplex encephalitis in multiple sclerosis? Case and discussion. Mult. Scler. Relat. Disord. 2, 385–387 (2013).
Shenoy, E. S., Mylonakis, E., Hurtado, R. M. & Venna, N. Natalizumab and HSV meningitis. J. Neurovirol. 17, 288–290 (2011).
Fine, A. J., Sorbello, A., Kortepeter, C. & Scarazzini, L. Central nervous system herpes simplex and varicella zoster virus infections in natalizumab-treated patients. Clin. Infect. Dis. 57, 849–852 (2013).
Fragoso, Y. D., Brooks, J. B., Gomes, S., de Oliveira, F. T. & da Gama, P. D. Report of three cases of herpes zoster during treatment with natalizumab. CNS Neurosci. Ther. 19, 280–281 (2013).
Gutwinski, S. et al. Severe cutaneous Candida infection during natalizumab therapy in multiple sclerosis. Neurology 74, 521–523 (2010).
Zecca, C., Nessi, F., Bernasconi, E. & Gobbi, C. Ocular toxoplasmosis during natalizumab treatment. Neurology 73, 1418–1419 (2009).
Desoubeaux, G. et al. Two cases of opportunistic parasite infections in patients receiving alemtuzumab. J. Clin. Pathol. 65, 92–95 (2012).
Author information
Authors and Affiliations
Contributions
A.W. and M.L. contributed equally to the manuscript. A.W. and M.L. drafted and wrote the manuscript, and all authors collected and reviewed literature. U.K.Z. and H.-P.H. drafted and critically revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
A.W. has received fees for speaking, consulting, serving on advisory boards and conducting clinical trials from Alexion, Bayer Healthcare, Biogen, Genzyme, Merck Serono, Novartis, Octapharma, Roche, Sanofi and Teva, with the approval of the Director of the University of Rostock Medical School. M.L. has received fees for speaking, consulting and conducting clinical trials from Abbvie, Astellas, GlaxoSmithKline, Gilead, Novartis Vaccines, Janssen and Roche, with the approval of the Director of the University of Rostock Medical School. E.C.R. has received speaker's honoraria, travel expense compensation and fees for conducting clinical trials from Activaero, Bayer, GlaxoSmithKline, Novartis Vaccines, Roche Pharma, and Sanofi Pasteur MSD, with approval from the Rector of the University of Rostock. H.-P.H. has received fees for consulting, speaking and serving on steering committees from Biogen, GeNeuro, Genzyme, Merck Serono, Novartis, Octapharma, Receptos, Roche, Sanofi and Teva, with approval from the Rector of Heinrich Heine University. U.K.Z has received fees for speaking, consulting, serving on advisory boards and conducting clinical trials from Bayer Healthcare, Biogen, Merck Serono, Novartis, Sanofi and Teva, with the approval of the Director of the University of Rostock Medical School.
Rights and permissions
About this article
Cite this article
Winkelmann, A., Loebermann, M., Reisinger, E. et al. Disease-modifying therapies and infectious risks in multiple sclerosis. Nat Rev Neurol 12, 217–233 (2016). https://doi.org/10.1038/nrneurol.2016.21
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2016.21
This article is cited by
-
Advising the immunocompromised traveller: a review of immunocompromise at The London Hospital for Tropical Diseases Travel Clinic between 1st April 2019 and 30th April 2020
Tropical Diseases, Travel Medicine and Vaccines (2024)
-
Key characteristics of anti-CD20 monoclonal antibodies and clinical implications for multiple sclerosis treatment
Journal of Neurology (2024)
-
Transcriptome alterations in peripheral blood B cells of patients with multiple sclerosis receiving immune reconstitution therapy
Journal of Neuroinflammation (2023)
-
Side effects following vaccination in multiple sclerosis: a prospective, multi-centre cohort study
Scientific Reports (2023)
-
Coronavirus disease 2019 (COVID-19) in pediatric patients with autoimmune disorders
European Journal of Pediatrics (2023)