Abstract
Aim The aim of this study is to quantify visual field defects after temporal lobectomy for mesial temporal sclerosis and to establish eligibility for driving.
Methods Automated static perimetry was performed on 14 patients who had undergone anterior temporal lobectomy for mesial temporal sclerosis. Perimetry consisted of monocular Humphrey Field Analyser (HFA) 30–2 test and a binocular Esterman 120 test.
Results Of the 14 patients, three had no loss or non-specific loss, eight had partial homonymous quadrantanopia, one had complete homonymous quadrantanopia and two had concentric loss attributable to vigabatrin, which may have masked any loss occurring due to surgery. Of these, only seven passed the standardised DVLA visual fields. Of the seven who failed DVLA visual field, one had complete quadrantanopia, four had partial quadrantanopia and two had concentric loss (due to vigabatrin).
Conclusions Visual field defects contribute a great deal in the reduction of the quality of life in patients who have had surgery for mesial temporal sclerosis. Potential surgically induced visual field defects that could preclude driving need to be discussed with each patient preoperatively. In our study 50% of patients did not meet the required DVLA standards.
Similar content being viewed by others
Introduction
The ability to drive has a great impact on modern day-to-day living. Surgery for intractable epilepsy aims to enhance the quality of life by rendering a patient seizure free; by virtue of this it gives the patient an opportunity to consider driving. Visual field defects in anterior temporal lobectomy have been well documented. In this study we have tried to establish the effects of visual field defects, after surgery, on the eligibility to drive as determined by specific standards laid down by the DVLA. The rule from the DVLA states:
‘The minimum field of vision for safe driving is defined as a field of at least 120° on the horizontal measured by the Goldmann perimeter using the III4e settings (or equivalent perimetry). In addition there should be no significant defect in the binocular field, which encroaches within 20° of fixation above or below the horizontal meridian. The DVLA requires a binocular Esterman field in the first instance to determine fitness to drive, and the false positive score must be no more than 20%. When a single missed point has been demonstrated within 20° of fixation on an Esterman binocular chart, this may represent a significant central defect and, in these circumstances, central charts should be undertaken. The standard is currently being rewritten in terms of the Esterman rather than the Goldmann’
Perimetry is a method of evaluating the visual field; it involves the presentation of stimuli of varying luminance in the same position to obtain a vertical boundary of the visual field. Automated perimetry may be threshold or supra-threshold; the former assesses threshold luminance values of the patient at various locations in the visual field, whereas in the latter, stimuli are presented at luminance levels above threshold levels. The 30–2 test on the Humphrey Field Analyser is a threshold test, whilst the binocular Esterman test is a supra-threshold one.
Goldmann perimetry is kinetic perimetry as it involves the presentation of a moving stimulus from a non-seeing to a seeing area. Using different stimulus intensities a contour map of the visual field can be created.
Methods
The records of 116 patients who underwent surgery for epilepsy over a period of 10 years at The University Hospital of Wales, Cardiff, were obtained. Of these only those who had undergone anterior temporal lobectomy for radiologically and pathologically proven mesial temporal sclerosis and had documented preoperative visual fields (other than confrontation) were selected for this study. Eighteen patients who met the above criteria were identified, but only 14 agreed to take part in the study. Three out of these four have now relocated to a different region and hence were reluctant to travel. The fourth patient could not be contacted at all.
Each patient underwent refraction to determine best-corrected visual acuity for distance and near; a cover test was also performed together with a record of the stereopsis with the Wirt stereo test. Automated Static Perimetry was performed on the Humphrey Field Analyser and the visual fields were assessed by the central 30–2 test and the binocular Esterman test. If patients failed the Esterman visual field test, it was repeated, as it is well recognised that the test performance can improve with practice.1,2 Details of the patients’ pre- and postoperative seizure frequency, anti-epileptic drug intake—pre- and postoperative, the side and extent of the lobectomy and other neurological deficits were also documented. These details are beyond the scope of this text.
Results
In all 14 patients were studied (Table 1), mean age being 44 years (range 33–57 years); seven were male and seven female. Surgery was performed by or in the presence of a consultant neurosurgeon at The University Hospital of Wales, Cardiff. All patients were right handed. Seven patients had a right-sided anterior temporal lobectomy (m:f :: 4:3); and seven had left-sided surgery (m:f :: 3:4).
Best-corrected distance Snellen visual acuity in each eye of all patients was 6/12 or better. With both eyes open each patient could see at least 6/9, best-corrected vision, thus meeting the DVLA requirement with regard to visual acuity.
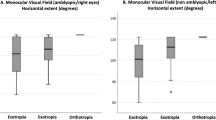
Stereopsis ranged from 1200 seconds of arc to 40 seconds of arc; with seven (50%) patients having 100 seconds of arc or better. Normal stereo acuity ranges from 40 to 60 seconds of arc. Two patients had stereopsis of 1200 seconds of arc and the cover test of these patients revealed an esophoria; these two patients also had reduced visual acuity in one eye accounting for poor stereo-acuity and hence suggestive of probable amblyopia.
A Goldmann visual field was performed in each case before surgery and was found to be full in all but two cases; these patients were on vigabatrin. All patients were followed for at least a year before the Humphrey Visual Fields were performed as a part of our study. The mean follow-up of the patients was 5.7 years (range 1–12 years).
On the 30–2 test, three (21%) patients were found to have normal visual field or non-specific loss; eight (57%) had partial quadrantanopia (Figure 1) and only one (7%) had complete quadrantanopia (Figure 2); concentric loss (Figure 3) was seen in two (15%) patients on vigabatrin, probably unchanged when compared to preoperative visual fields. However the pre- and postoperative visual fields in this study are not strictly comparable as the former were performed using kinetic perimetry (Goldmann), and static perimetry (Humphrey) was used for the latter. Driving fields as assessed using the binocular Esterman test demonstrated that seven (50%) out of 14 patients met the current visual field criteria as specified by the DVLA. Of the seven who failed the DVLA visual field, one had complete quadrantanopia, four had partial quadrantanopia and two had concentric loss (due to vigabatrin).
None of the patients had a false positive score of greater than 11%, where up to 20% is allowed by the DVLA. Patients failing the Esterman visual field test twice had their results substantiated by the monocular Humphrey 30–2 test which in all cases confirmed the visual field loss.
Discussion
The presence of visual field defects after anterior temporal lobectomy has been well documented.3,4,5,6,7,8,9 In this operation, anterior and inferiormost fibres of the geniculo-calcarine tract, Meyer’s loop, are most vulnerable to damage in their course around the temporal horn of the lateral ventricle;3,5 the variation in its anatomical pathway makes it possible to have varying degrees of visual field defects even when the same operation is performed by the same surgeon for the same pathology. Krolak-Salmon et al have concluded that the anterior limit of Meyer’s loop is likely to be located more rostrally than previously believed.5
Our study concentrates on visual field defects after anterior temporal lobectomies for mesial temporal sclerosis only, and its effects on driving. We recorded a visual field defect in 11 out 14 (79%) patients on the monocular 30–2 Humphrey field analyser. Of these patients with visual field defects, two out of 14 (18%) were attributed wholly or partially to use of vigabatrin,4,10 as typical concentric visual field defect was noted both pre- and postoperatively. Our finding of a visual field defect in 79% of patients compares favourably to other studies done with automated static perimetry. Krolak-Salmon et al describe a visual field defect of 83.3% with automated static perimetry and Hughes et al3 describe a visual field defect in 31 out of 32 (97%) patients when tested with the Humphrey 30–2 test. Falconer and Wilson report a defect in 100% of patients in a series of horizontal sections of the temporal lobe varying from 45–90 mm from the temporal lobe tip. Visual field defects as detected by automated perimetry are more than those previously reported6,7 and are probably due to the fact that automated static perimetry is by far a more sensitive test in picking up smaller defects than kinetic perimetry.
The two patients in our study who were on vigabatrin failed the visual field test as they had bilateral concentric constriction of visual field with relative sparing of the temporal field.4,10
Moreover, inspite of 79% of patients having visual field defects, only 50% failed their driving field tests according to the DVLA criteria. One of the major drawbacks of the DVLA visual field test is the profound demonstrated learning effect.1,2 The DVLA guidelines also do not stipulate the number of tests that a person can undertake. Patients failing the test, therefore, had the test repeated, with at least once on a separate day, to help eliminate both patient fatigue and learning effect. In our study nine patients had originally failed the test, but subsequently two patients passed on repeated testing. We are not aware of any other study that assesses driving in this particular group of patients. The study by Manji et al6 did compare Goldmann and Esterman perimetry with regards to driving in a heterogeneous group of 24 patients undergoing temporal lobectomy, including those with mesial temporal sclerosis. They found 42% failed the driving requirements with the monocular Goldmann test and only 24% failed with the binocular Esterman test. This difference may be attributed to the heterogeneity of the group and selection bias of the study itself.
Conclusions
Visual field defects contribute significantly to the postoperative morbidity in patients who have had surgery for mesial temporal sclerosis. This may cause significant distress to patients who are seizure free, but find that they are unable to drive because of the visual field defects. The probability of visual field defects should be discussed at length before surgery to avoid disappointment afterwards. Surprisingly only 50% had visual field defects that prevented driving. Based on this study, patients can be counselled preoperatively of the risks of visual field defects that could prevent them from driving.
References
Heijl A, Lindgren G, Olsson J . The effect of perimetric experience in normal subjects. Arch Ophthalmol 1989; 107: 81–86
Wood JM, Wild JM, Hussey MK, Crews SJ . Serial examination of the normal visual field using Octopus automated projection perimetry. Evidence for a learning effect. Acta Ophthalmol (Copenh) 1987; 65: 326–333
Hughes TS, Abou-Khalil B, Lavin PJ, Fakhoury T, Blumenkopf B, Donahue SP . Visual field defects after temporal lobe resection: a prospective quantitative analysis. Neurology 1999; 53: 167–172
Hardus P, Verduin WM, Postma G, Stilma JS, Berendschot TT, van Veelen CW . Long term changes in the visual fields of patients with temporal lobe epilepsy using vigabatrin. Br J Ophthalmol 2000; 84: 788–790
Krolak-Salmon P, Guenot M, Tiliket C, Isnard J, Sindou M, Mauguiere F et al. Anatomy of optic nerve radiations as assessed by static perimetry and MRI after tailored temporal lobectomy. Br J Ophthalmol 2000; 84: 884–889
Manji H, Plant GT . Epilepsy surgery, visual fields, and driving: a study of the visual field criteria for driving in patients after temporal lobe epilepsy surgery with a comparison of Goldmann and Esterman perimetry. J Neurol, Neurosurg Psychiatry 2000; 68: 80–82
Tecoma ES, Laxer KD, Barbaro NM, Plant GT . Frequency and characteristics of visual field deficits after surgery for mesial temporal sclerosis. Neurology 1993; 43: 1235–1238
Jensen I, Seedorff HH . Temporal lobe epilepsy and neuro-ophthalmology. Ophthalmological findings in 74 temporal lobe resected patients. Acta Ophthalmologica 1976; 54: 827–841
Katz A, Awad IA, Kong AK, Chelune GJ, Naugle RI, Wyllie E et al. Extent of resection in temporal lobectomy for epilepsy. II. Memory changes and neurologic complications. Epilepsia 1989; 30: 763–771
Hardus P, Verduin WM, Postma G, Stilma JS, Berendschot TT, van Veelen CW . Concentric contraction of the visual field in patients with temporal lobe epilepsy and its association with the use of vigabatrin medication. Epilepsia 2000; 41: 581–587
Acknowledgements
We thank J Wild, Professor of Optometry, University of Wales, Cardiff, for his help in the interpretation of visual fields.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pathak-Ray, V., Ray, A., Walters, R. et al. Detection of visual field defects in patients after anterior temporal lobectomy for mesial temporal sclerosis—establishing eligibility to drive. Eye 16, 744–748 (2002). https://doi.org/10.1038/sj.eye.6700152
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700152
Keywords
This article is cited by
-
Cross-subject variability of the optic radiation anatomy in a cohort of 1065 healthy subjects
Surgical and Radiologic Anatomy (2023)
-
Fractional anisotropy of the optic radiations correlates with the visual field after epilepsy surgery
Neuroradiology (2019)
-
Visual field deficits after epilepsy surgery: a new quantitative scoring method
Acta Neurochirurgica (2018)
-
Direct electrical stimulation of the optic radiation in patients with covered eyes
Neurosurgical Review (2014)
-
Navigated three-dimensional intraoperative ultrasound-guided awake resection of low-grade glioma partially infiltrating optic radiation
Acta Neurochirurgica (2012)