Summary
Abstract
Rivastigmine (SDZ ENA 713) is a carbamylating, long-acting reversible and noncompetitive carbamate acetylcholinesterase inhibitor that is indicated as an oral treatment for patients with mild to moderately severe Alzheimer’s disease. The drug has been evaluated for this use in 3 well designed, adequately powered, phase II/III, 26-week clinical trials that included a total of 1479 rivastigmine and 647 placebo recipients. Most of these patients had concomitant disorders that were being treated with numerous other drugs.
Individual and pooled results of these trials indicate that rivastigmine 6 to 12 mg/day usually produces cognitive, global and functional changes that indicate significantly less deterioration than was observed with placebo in patients with mild to moderately severe Alzheimer’s disease. Individual results of the 2 pivotal trials and pooled analysis also show that, compared with placebo recipients, significantly more rivastigmine 6 to 12 mg/day recipients respond to therapy. Indeed, after 26 weeks of therapy in the 2 pivotal trials, significantly more rivastigmine 6 to 12 mg/day than placebo recipients achieved clinically meaningful improvements as defined by 3 separate response criteria. The lower dosage range of 1 to 4 mg/day was not as effective as 6 to 12 mg/day, as measured using these criteria and other efficacy parameters.
Rivastigmine causes adverse events that are generally those expected from an acetylcholinesterase inhibitor. They are usually mild to moderate, of short duration and responsive to dosage reduction. Unpublished data from 3989 patients indicate that rivastigmine and placebo were associated with similar incidences of serious adverse events and changes in laboratory parameters, ECG and cardiorespiratory vital signs. The most common events were gastrointestinal, central and peripheral nervous system and whole body adverse events. However, compared with placebo, rivastigmine more commonly caused adverse events resulting in treatment withdrawal. These events were most frequently gastrointestinal and were more common in women.
Conclusion:Rivastigmine is a useful option for the treatment of patients with mild to moderately severe Alzheimer’s disease. Although only short term (6-month) comparisons with placebo are available, given the lack of established treatment options it should be considered for first-line use in this population.
Introduction
Alzheimer’s disease is one of the most disabling conditions that affects the elderly and, until recently, was considered untreatable. It affects about 17 to 25 million people worldwide and death is expected within 7 to 10 years of diagnosis. The aetiology and pathogenesis of Alzheimer’s disease have not been well established. However, a number of factors, including age and neurotransmitter deficits, are thought to contribute to development of the disease.
The cognitive deficits seen in patients with Alzheimer’s disease are attributed to degeneration of cholinergic pathways. Thus, palliative therapy for patients with Alzheimer’s disease has revolved around restoring cholinergic function. Several strategies have been employed, the most successful of which has been use of cholinesterase inhibitors.
Pharmacodynamic Properties
Rivastigmine inhibits acetylcholinesterase less potently than physostigmine in vitro and in vivo (in rats). However, unlike physostigmine, rivastigmine has selectivity for the hippocampus and cortex (rather than the striatum and pons/medulla) in the brain, and selectivity for the brain (rather than the heart or skeletal muscle) in rats. This increased inhibitory activity in the hippocampus and cortex, which are the areas of the brain most affected by Alzheimer’s disease, may result from preferential activity at the globular G1 form of acetylcholinesterase. Rivastigmine has no affinity for muscarinic, α- or β-adrenergic, dopaminergic or opioid receptors.
Results of studies conducted in animal models indicate that rivastigmine has central cholinergic activity, but little peripheral activity. The ratio of central to peripheral cholinergic effects was about 5 times greater than that of physostigmine.
CSF acetylcholinesterase and butyrylcholinesterase activity is dose-dependently reduced by rivastigmine 1 to 6mg twice daily in patients with Alzheimer’s disease. Significant inhibition of acetylcholinesterase is maintained for up to 11.6 hours (with the 6mg twice daily dosage). Inhibition of butyrylcholinesterase activity in the plasma is numerically lower than in the CSF at all dosage levels and inhibition of this enzyme is generally more variable than inhibition of acetylcholinesterase.
In old rats, rivastigmine increased depressed acetylcholine levels and choline acetyltransferase activity to levels found in younger rats. Reductions in choline acetyltransferase activity in basal forebrain-lesioned rats were also attenuated by rivastigmine, but not tacrine or physostigmine. Rivastigmine increased the number of muscarinic M1 receptor binding sites in the frontal cortex of aged rats and attenuated the decreases in cortical muscarinic acetylcholine receptor binding ability (without changes in binding affinity) seen in aged rats.
Rivastigmine attenuated spatial memory and/or learning impairment induced by basal forebrain lesions in rats as shown in the water maze test and a step-down avoidance paradigm.
Rivastigmine demonstrated no abuse potential and did not cause physical dependence in rhesus monkeys.
Pharmacokinetic Properties
Published pharmacokinetic data for rivastigmine are scant, although unpublished data from patients (625 patients enrolled in phase II/III trials) and volunteers are available.
After oral administration, rivastigmine is rapidly absorbed and extensively biotransformed to the decarbamylated metabolite NAP 226-90 (ZNS 114-666) which is soon detected in the CSF [time (tmax) to CSF maximum concentration (Cmax) of 1.4 to 3.8 hours]. In patients, plasma and CSF Cmax values and areas under the concentration-time curves for the first 12 hours (AUC12) for both rivastigmine and NAP 226-90 are significantly correlated with oral dose. Concomitant food slows the absorption of rivastigmine and results in a decrease in Cmax values of approximately 30% and an increase in AUC values of about 30%.
Systemic exposure to rivastigmine is not affected by age, but drug concentrations are inversely related to body surface area and nicotine consumption. Concentrations of NAP 226-90 are also inversely related to body surface area. Cholinergic adverse events, such as anorexia, diarrhoea, nausea and vomiting, are correlated more with NAP 226-90 than rivastigmine concentrations. Inhibition of acetylcholinesterase activity tends to be directly related to CSF rivastigmine and NAP 226-90 concentrations.
Rivastigmine is rapidly and extensively metabolised, primarily by cholinesterases, to NAP 226-90. NAP 226-90 may then undergo N-demethylation and/or sulphate conjugation. After metabolism, rivastigmine undergoes rapid renal elimination. Repeated administration of rivastigmine (1 to 6mg twice daily) does not result in accumulation of the parent drug or NAP 226-90.
Coexisting hypertension, dyspepsia, diabetes mellitus, arthritis or neoplasia do not significantly affect plasma concentrations of rivastigmine or NAP 226-90. Age does not consistently affect the absorption of rivastigmine, but elimination is slightly prolonged in the elderly. As the metabolism of rivastigmine and elimination of NAP 226-90 appear to be reduced in patients with renal and mild to moderate hepatic impairment, dosage recommendations to titrate according to individual tolerability should be closely followed in these patients. Patients with severe hepatic impairment have not been studied.
Because rivastigmine is poorly plasma protein bound and its metabolism is mediated predominantly by esterases rather than hepatic microsomal (cytochrome P450) enzymes, clinically relevant drug interactions are unlikely. In vitro and kinetic studies conducted in patients receiving a variety of agents support this assumption. However, interactions with drugs that have an effect on the cholinergic system may occur.
Clinical Efficacy
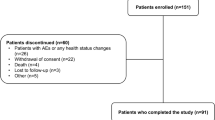
Rivastigmine has been evaluated for the treatment of mild to moderately severe Alzheimer’s disease in 3 well designed, adequately powered, phase II/III, 26-week clinical trials (total n = 2126). Individual and pooled results of these trials generally indicate that rivastigmine 6 to 12 mg/day produced significantly less cognitive, global and functional deterioration than was seen with placebo in patients with mild to moderate Alzheimer’s disease. Activities of daily living were also significantly better in rivastigmine 6 to 12 mg/day recipients than in the placebo group in the 2 pivotal trials.
Pooled analysis of these trials and individual results of the 2 pivotal trials also showed that, compared with placebo recipients, significantly more rivastigmine 6 to 12 mg/day recipients responded to therapy. Indeed, at 26 weeks, significantly more rivastigmine 6 to 12 mg/day than placebo recipients achieved clinically meaningful improvements as defined by 3 separate sets of criteria: a ≥4-point improvement for Alzheimer’s Disease Assessment Scale — Cognitive subscale (ADAS-Cog) scores, a ≥10% improvement for the Progressive Deterioration Scale (PDS) score and a rating of <4 for the Clinician’s Interview Based Impression of Change — Plus (CIBIC-Plus). Significant benefits for rivastigmine were also seen at weeks 12 and 18.
In the pooled analysis and 1 pivotal trial, rivastigmine 1 to 4 mg/day demonstrated some benefits over placebo, but this dosage range was not as effective, according to primary and secondary end-points, as the 6 to 12 mg/day range (in most instances no statistical analysis was provided between dosages).
Results of an additional phase II/III trial which enrolled 702 patients also showed that recipients of rivastigmine 6 or 9 mg/day had significantly less deterioration according to ADAS-Cog scores than did placebo recipients at week 26. However, changes in the other primary end-point (CIBIC-Plus) and secondary end-points generally were not significantly different from those seen with placebo and the proportion of responders in each rivastigmine treatment group did not usually differ from that in the placebo group. This trial differed in methodology from the other phase II/III trials in that, after dose titration, patients received a fixed dosage of rivastigmine.
Rivastigmine appears more effective in older patients (≥75 years), nonsmokers and those with a higher baseline ADAS-Cog score and lower bodyweight. It has its greatest effects on symptoms associated with short term memory. Tolerance to the therapeutic effects of rivastigmine does not occur.
Tolerability
Adverse events observed with rivastigmine are generally those expected from an acetylcholinesterase inhibitor. They are usually mild to moderate, of short duration and either respond to dosage reduction or resolve spontaneously. Most patients (85%) receiving rivastigmine in clinical trials had concomitant disorders that were being treated with numerous drugs.
Unpublished tolerability data from 3006 patients who received rivastigmine in clinical trials (>200 received the drug for 1 year and >1200 were treated for ≥6 months) indicate that the incidences of serious adverse events or changes in laboratory parameters, ECG and cardio-respiratory vital signs were not significantly different with rivastigmine and placebo. The majority of adverse events were cholinergically mediated and the most common were gastrointestinal. The next most frequently reported events were central and peripheral nervous system and whole body adverse events.
Rivastigmine more commonly caused adverse events resulting in treatment withdrawal than did placebo. These events were most frequently gastrointestinal and were more common in women.
The most common adverse event, nausea, was more likely to occur during the dose titration period than during other treatment times. Nausea resolved in 85% of patients, usually following dosage reduction. As with other cholinesterase inhibitors, rivastigmine is associated with weight loss. For example, clinically notable weight loss (≥7%) occurred in 21% of rivastigmine 6 to 12 mg/day recipients and 2% of placebo recipients in 1 clinical trial.
Of the serious adverse events reported in clinical trials, only gastrointestinal haemorrhage, angina pectoris and syncope were more common with rivastigmine than with placebo. Overdosage with rivastigmine resulted in mild to moderate nausea, vomiting and diarrhoea which usually resolved spontaneously.
Evaluation of 197 patients who completed 1 year of treatment with rivastigmine indicates that the most common emergent adverse events of long term treatment with rivastigmine were gastrointestinal (nausea, anorexia, vomiting and diarrhoea).
Dosage and Administration
Oral rivastigmine should be started at a dosage of 1.5mg twice daily for a minimum of 2 weeks. After this time, the dosage can be titrated upwards, preferably at intervals of ≥2 weeks, to 6 mg/day or higher depending on development of dose-limiting adverse events. Patients should receive the highest tolerated dosage up to a maximum of 12 mg/day, administered as 2 equally divided daily doses. It is recommended that rivastigmine be taken with food to reduce the risk of adverse events. The drug should not be given to patients with severe hepatic impairment as it is yet to be studied in this population.
Similar content being viewed by others
References
American Psychiatric Association. Practice guideline for the treatment of patients with Alzheimer’s disease and other dementias of late life. Am J Psychiatry 1997 May; 154 Suppl.: 1–39
Jaen JC, Davis RE. Cholinergic therapies for Alzheimer’s disease: acetylcholinesterase inhibitors of current clinical interest. Curr Opin Invest Drug 1993 Apr; 2: 363–77
Eagger SA, Harvey RJ. Tacrine and other anticholinesterase drugs in dementia. Curr Opin Psychiatry 1995 Jul; 8: 264–7
Parnetti L, Senin U, Mecocci P. Cognitive enhancement therapy for Alzheimer’s disease: the way forward. Drugs 1997 May; 53: 752–68
Thal LJ, Carta A, Doody R, et al. Prevention protocols for Alzheimer disease: position paper from the International Working Group on Harmonization of Dementia Drug Guidelines. Alz Dis Assoc Disord 1997; 11Suppl. 3: 46–9
Lamy PP. The role of cholinesterase inhibitors in Alzheimer’s disease. CNS Drugs 1994 Feb; 1: 146–65
Enz A, Amstutz R, Boddeke H, et al. Brain selective inhibition of acetylcholinesterase: a novel approach to therapy for Alzheimer’s disease. Prog Brain Res 1993; 98: 431–8
Lawrence AD, Sahakian BJ. Alzheimer disease, attention, and the cholinergic system. Alz Dis Assoc Disord 1995; 9Suppl. 2: 43–9
Guillozet AL, Smiley JF, Mash DC, et al. Butyrylcholinesterase in the life cycle of amyloid plaques. Ann Neurol 1997; 42: 909–18
Sadoshima S, Ibayashi S, Fujii K, et al. Inhibition of acetylcholinesterase modulates the autoregulation of cerebral blood flow and attenuates ischemic brain metabolism in hypertensive rats. J Cereb Blood Flow Metab 1995 Sep; 15: 845–51
Tanaka K, Ogawa N, Asanuma M, et al. Effects of the acetylcholinesterase inhibitor ENA-713 on ischemia-induced changes in acetylcholine and aromatic amine levels in the gerbil brain. Arch Int Pharmacodyn Ther 1993 May–Jun; 323: 85–96
Tanaka K, Mizukawa K, Ogawa N, et al. Post-ischemic administration of the acetylcholinesterase inhibitor ENA-713 prevents delayed neuronal death in the gerbil hippocampus. Neurochem Res 1995 Jun; 20: 663–7
Chen Y, Shohami E, Bass R, et al. Cerebro-protective effects of ENA713, a novel acetylcholinesterase inhibitor, in closed head injury in the rat. Brain Res 1998; 784: 18–24
Enz A, Boddeke H, Gray J, et al. Pharmacologic and clinico-pharmacologic properties of SDZ ENA 713, a centrally selective acetylcholinesterase inhibitor. Ann N Y Acad Sci 1991; 640: 272–5
Weinstock M, Razin M, Chorev M, et al. Pharmacological evaluation of phenyl-carbamates as CNS-selective acetylcholinesterase inhibitors. J Neural Transm 1994; 43 Suppl.: 219–25
Cutler NR, Polinsky RJ, Sramek JJ, et al. Dose-dependent CSF acetylcholinesterase inhibition by SDZ ENA 713 in Alzheimer’s disease. Acta Neurol Scand 1998; 97: 244–50
Tanaka K, Ogawa N, Asanuma M, et al. Chronic administration of acetylcholinesterase inhibitor in the senescent rat brain. Neurobiol Aging 1994 Nov–Dec; 15: 721–5
Ohara T, Tanaka K-i, Fukaya H, et al. Different profile of SDZ ENA 713 from other acetylcholinesterase inhibitors to improve cholinergic deficit in basal forebrain-lesioned rats [abstract no. P-158]. Jpn J Pharmacol 1996; 71Suppl. I: 98P
Tanaka K-i, Oh-hara T, Fukaya H, et al. Effects of SDZ ENA-713 on choline acetyltransferase activity and muscarinic acetylcholine receptor binding in the brains of learning impaired rats [abstract no. P3-237]. Jpn J Pharmacol 1995; 67Suppl. I: 306P
Oh-hara T, Tanaka K-i, Fukaya H, et al. Effects of SDZ ENA 713 on spatial memory impairment in basal forebrainlesioned rats [abstract no. P-652]. Jpn J Pharmacol 1994; 64Suppl. 1: 353P
Niigawa H, Tanimukai S, Takeda M, et al. Effects of SDZ ENA 713, novel acetyl cholinesterase inhibitor, on learning of rats with basal forebrain lesions. Prog Neuropsych Biol Psychiatry 1995 Jan; 19: 171–86
Holsboer-Trachsler E, Hatzinger M, Stohler R, et al. Effects of the novel acetylcholinesterase inhibitor SDZ ENA 713 on sleep in man. Neuropsychopharmacology 1993 Jan; 8: 87–92
Anand R. Clinical expert report: Exelon/Alzheimer’s disease. Basle, Switzerland: Novartis Pharma AG, 1997. (Data on file)
Stadtmüller G, Bahro M, Riemann D, et al. The impact of the novel acetylcholine esterase inhibitor SDZ ENA 713 on sleep EEG in Alzheimer’s disease and old age depression [abstract no. O-168-229]. Neuropsychopharmacology 1994 May; 10 (Pt 2) Suppl.: 58S
Kelly PH, Amstutz R, Enz A. Assessment of the abuse potential of the novel cholinesterase inhibitor SDZ ENA 713 in the rhesus monkey [abstract]. Nida Res Monogr Ser 1993; (132): 245
Polinsky RJ. Clinical pharmacology of rivastigmine: a new-generation acetylcholinesterase inhibitor for the treatment of Alzheimer’s disease. Clin Ther 1998; 20(4): 634–47
Integrated summary of effectiveness. SNZ ENA 713 capsules: probable Alzheimer’s disease. Novartis Pharmaceuticals Corporation (New Jersey). Sep 8, 1997. (Data on file)
Corey-Bloom J, Anand R, Veach J, et al. A randomized trial evaluating the efficacy and safety of ENA 713 (rivastigmine tartrate), a new acetylcholinesterase inhibitor, in patients with mild to moderately severe Alzheimer’s disease. Int J Geriatr Psychiatry 1998; 1: 55–65
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association, 1994
McKhann G, Drachman D, Folstein M, et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 1984; 34: 939–44
Rösler M, Anand R, Cicin-Sain A, et al. Safety and efficacy of rivastigmine (Exelon®) in patients with Alzheimer’s disease: results of an international, 26-week, multicentre, randomised, placebo-controlled trial. BMJ. In press
Anand R, Gharabawi G, Enz A. Efficacy and safety results of the early phase studies with Exelon™ (ENA-713) in Alzheimer’s disease: an overview. J Drug Dev Clin Pract 1996 Sep; 8: 109–16
Ferris SH, Lucca U, Mohs R, et al. Objective psychometric tests in clinical trials of dementia drugs: position paper from the International Working Group on Harmonization of Dementia Drug Guidelines. Alz Dis Assoc Disord 1997; 11Suppl. 3: 34–8
Anand R, Gharabawi G. Clinical development of Exelon™ (ENA-713): the ADENA® programme. J Drug Dev Clin Pract 1996 Sep; 8: 117–22
Stern RG, Mohs RC, Davidson M, et al. A longitudinal study of Alzheimer’s disease: measurement, rate, and predictors of cognitive deterioration. Am J Psychiatry 1994; 151(3): 390–6
Rosen WG, Mohs RC, Davis KL. A new rating scale for Alzheimer’s disease. Am J Psychiatry 1984; 141(11): 1356–64
Solomon PR, Knapp MJ, Gracon SI, et al. Long-term tacrine treatment in patients with Alzheimer’s disease [letter]. Lancet 1996 Jul 27; 348: 275–6
Antuono PG, for The Mentane Study Group. Effectiveness and safety of velnacrine for the treatment of Alzheimer’s disease. A double-blind, placebo-controlled study. Arch Intern Med 1995; 155: 1766–72
Rogers SL, Farlow MR, Doody RS, et al. A 24-week, double-blind, placebo-controlled trial of donepezil in patients with Alzheimer’s disease. Neurology 1998; 50: 136–45
Knapp MJ, Knopman DS, Solomon PR, et al. A 30-week randomized controlled trial of high-dose tacrine in patients with Alzheimer’s disease. JAMA 1994 Apr 6; 271(13): 985–91
Thal LJ, Carta A, Clarke WR, et al. A 1-year multicenter placebo-controlled study of acetyl-L-carnitine in patients with Alzheimer’s disease. Neurology 1996; 47: 705–11
Rogers SL, Doody RS, Mohs RC, et al. Donepezil improves cognitive and global function in Alzheimer Disease. A 15-week, double-blind, placebo-controlled study. Arch Intern Med 1998; 158: 1021–31
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spencer, C.M., Noble, S. Rivastigmine. Drugs Aging 13, 391–411 (1998). https://doi.org/10.2165/00002512-199813050-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002512-199813050-00005